ʴकชʵ
%
%LRPHFKDQLFDO DQDO\VLV RI PHGLDO SDWHOORIHPRUDO OLJDPHQW UHFRQVWUXFWLRQ )LEHU7DSHZLWKNQRWOHVVDQFKRUVYHUVXVDVHPLWHQGLQRVXVWHQGRQDXWRJUDIWZLWKVRIW DQFKRUV
ʤ಼ଈග֘Ḳਡଵ࠸ݒͶ͕͜Ζਫ਼ରྙָదࢾݩ
ʗ)LEHU7DSH ͳόρφϪηΠϱΩʖόρφϪηΠϱΩʖΝ༽͏ͪढ़ࣞͳ ൔ伵༹۔伵ͳλϓφΠϱΩʖΝ༽͏ͪढ़ࣞർֳʗʥ
ਅ ੧ ं ߄ָָӅҫָݜڂՌ ؽ࠸ݒʀ࠸ਫ਼ՌָҮ
ӣಊؽබସरָگүݜڂ
ࢱ ໌ ሥ ഇ ༬
ࢨگद ੶ ڰ ڭ ೯
ABSTRACT
Background: With the use of synthetic materials for medial patellofemoral ligament (MPFL) reconstruction, graft harvest is not necessary and this may facilitate post- operative rehabilitation. The purpose of this study was to compare the structural properties of MPFL reconstruction using a modern synthetic material (FiberTapeۑ5 (FT), Arthrex) with knotless anchors or a semitendinosus (ST) tendon autograft with soft anchors.
Methods: Nine human fresh-frozen amputated knees were used in this study. After the tensile strength of the native MPFL was measured, the MPFLs were reconstructed using two different surgical procedures, FT with knotless anchors (group A) and a ST with soft anchors (group B). Mechanical testing to failure of the reconstructed MPFLs was performed, and the ultimate load (N), stiffness (N/mm), and failure mode were recorded.
Results: The mean (± standard deviation) ultimate load of the native MPFL was 130.6 ± 28.7 N, and all native MPFLs failed at the femoral insertion site. Ultimate load of group A was significantly higher than that of the native MPFL (175.9 ± 34.1 N, p < 0.05). In contrast, the ultimate load of group B was significantly lower than that of the native MPFL (102.7 ± 21.4 N, p < 0.05). The mean stiffness was significantly higher for MPFLs in group A (17.4 ± 4.3 N/mm) than in group B (8.5 ± 1.8 N/mm, p < 0.05). In group A, 5
specimens failed via a knotless anchor pullout at the femoral side, 3 via pullout of knotless anchors at the patella side and 1 via fracture (cheese cut) of the femur without breakage of knotless anchor. In group B, all specimens failed via soft anchor pullout at the patella side. There was no incidence of rupture of FT or ST.
Conclusion: FT with knotless anchors was stronger than a ST with soft tissue anchors for MPFL reconstruction.
Introduction
The medial patellofemoral ligament (MPFL) plays an important role in patellar stability, providing 50% to 60% of the total medial restraining force on the patella from 0° to 30° of knee flexion (1). Clinically, the MPFL is ruptured after acute dislocation of the patella with a probability of recurrent patellar dislocation of 13% to 50% (2). Patellar dislocation is managed non-operatively at first (3), with the aim of decreasing swelling, promoting greater activation of vastus medialis obliquus and gluteal, and increasing the range of motion of the knee (4). However, conservative treatment is associated with rates of re-dislocation as high as 63% (5).
MPFL reconstruction is one of operative procedures in patients with recurrent dislocations. There are a variety of devices and techniques such as interference screw, suture anchor, and through tunnel or double tunnel technique, available for fixation of a graft to the anatomic insertion site of the MPFL. Regardless of the fixation device or technique, some surgeons use artificial ligament for the graft (6), and others use autologous tendon graft (7-10). We have used a semitendinosus tendon (ST) with soft anchors (FiberTak Suture Anchor, Arthrex, Naples, Florida) for MPFL reconstruction. In this surgical procedure, soft anchors potentially decreased the risk for patella fracture and violation of the articular surface (11), however autologous tendon graft had a possibility
of stretching over time and a risk of donor site damage such as neurovascular injury. On the other hand, artificial ligament is more rigid than autograft, and it is important not to overtighten the fixation construct at the time of surgery (12). Recently, Lee et al. (12) reported the use of a synthetic material (FiberTapeۑ5 (FT), Arthrex) with knotless anchors for MPFL reconstruction. According to their report, FT is a safe and effective alternative for MPFL reconstruction and tendon harvesting is unnecessary for optimal results which reduce the risks associated with the donor site (12). Bisson et al (13) reported that tensile strength of FT is 937 ± 93 N, and it was considered that FT had sufficient tensile strength for MPFL reconstruction. However, to our knowledge, there are no studies about the biomechanics of MPFL reconstruction using FT with knotless anchors.
The purpose of this study was to compare the structural properties of MPFL reconstruction using FT with knotless anchors, and the ST with soft anchors that we had used for MPFL reconstruction until now. Our hypothesis was that FT with knotless anchors provides sufficient strength for MPFL reconstruction.
Materials and Methods
Nine fresh-frozen male human amputated knees, with a mean patient age of 65.8
± 5.2 years (49-73) at the time of amputation, that were donated to our university for
anatomical study, were used. Informed consent was obtained from the patients. Ethical approval of this study was obtained from the ethics committee of our institute. Specimens with prior surgery, abnormal laxity, or osteoarthritis were excluded.
Specimen preparation
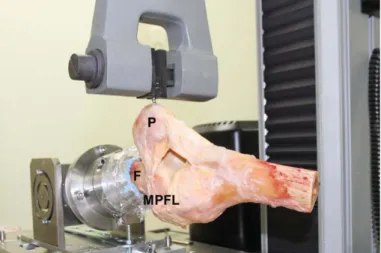
Specimens were stored at -20° and then thawed at room temperature 24 hours before testing. Specimens were kept moist with saline solution irrigation throughout the preparation and mechanical testing. ST were harvested and prepared for the grafts. All soft-tissue structures were removed to expose the femur and tibia, with knee ligaments, posterior structures, and extensor mechanism being left intact. Then, the MPFL was dissected carefully, as described by Nomura (14), and kept intact. The medial retinaculum, except for the MPFL, lateral retinaculum, and joint capsule were removed. The proximal part of the femur was placed in a custom-made metallic pot with polymethyl methacrylate for attachment to a material testing machine (Instron 4465, Instron, Canton, MA), and a 4.5-mm cancellous screw was inserted into the lateral ridge of patella for attachment to the crosshead of the Instron. In order to reproduce a lateral dislocation of the patella, the femur was mounted horizontally with the lateral femoral condyle positioned upward, and the cancellous screw was firmly gripped with the crosshead (Figure 1).
MPFL reconstruction
MPFL reconstruction was performed using two different surgical procedures: FT with knotless anchors (group A) and ST with soft anchors (group B). In group A, the central portion of FT was fixed by two 3.5-mm knotless anchors (PEEK SwiveLock® C Vented, Arthrex) on the medial border of the patella. Then, the two free ends of the FT were fixed using a 4.75-mm knotless anchor (PEEK SwiveLock® C Vented, Arthrex) on the femoral side while the patella was kept in the center of the patellar groove with the knee in 60° of flexion (Figure 2-A). In group B, a harvested ST was used for MPFL reconstruction, and was fixed using two soft anchors on the medial border of the patella, and fixed using a 7-mm interference screw (ThreadTight Interference Screw, Arthrex Japan) on the femoral side (Figure 2-B). For femoral fixation of the ST, a 6.0-mm diameter tunnel was created at the MPFL insertion, and the two free ends of the ST were pulled into this tunnel and fixed by the interference screw, under the same condition as for group A. After testing of the native MPFL, the order of reconstruction for each specimen was randomly allocated. After the first reconstructive devices were removed, the second procedure was performed, with care taken to place the fixation sites on the patella and femoral side 5-10 mm apart from the previous sites to maintain a sufficient bone bridge.
Biomechanical testing
The patella was placed at the center of the patellar groove,with the knee in a reference position of 60° of flexion throughout the testing, and 10 cycles of a lateral pulling force (± 1 N) was applied for preconditioning of the MPFL (15). Following this preconditioning, the biomechanical testing of the intact MPFL was performed under a crosshead speed of 10 mm/min. The load-displacement curve was recorded at 200 Hz until failure. The ultimate tensile load was considered to be the peak force. Stiffness was calculated by using a best-fit line to determine the slope of the linear portion of the load- displacement curve. Ultimate load (N) and stiffness (N/mm), and the failure mode of intact MPFL were recorded. The same biomechanical tests were repeated after each MPFL reconstruction procedure.
Statistical analysis
The mean values of ultimate load and stiffness for the native MPFL and reconstructed MPFLs (groups A and B) were compared using an analysis of variance and Tukey’s post hoc tests. Data input and analyses were performed using SPSS (version 12.0J, SPSS Inc., Chicago, IL, USA). A P-value <0.05 was considered statistically significant.
Results
The mean (± standard deviation, SD) ultimate load and stiffness of the native
MPFL were 130.6 ± 28.7 N and 12.0 ± 3.7 N/mm, respectively. All native MPFL failed at the femoral insertion site. The mean (± SD) ultimate load for the reconstructed MPFL in groups A and B were 178.4 ± 4.4 N and 102.8 ± 21.5 N, respectively. The mean ultimate load of group A MPFLs was significantly higher than that of the native (p=0.038) and group B (p<0.001) MPFLs (Figure 3).
The mean stiffness of group A and B MPFLs were 17.4 ± 4.3 N/mm and 8.5 ± 1.8 N/mm, respectively. The mean stiffness of the group A MPFL was significantly higher than for MPFLs in group B (p=0.001; Figure 4). Although there was no significant difference between the native MPFL and group B MPFLs, both ultimate load and stiffness of group B were lower than those of the native MPFL.
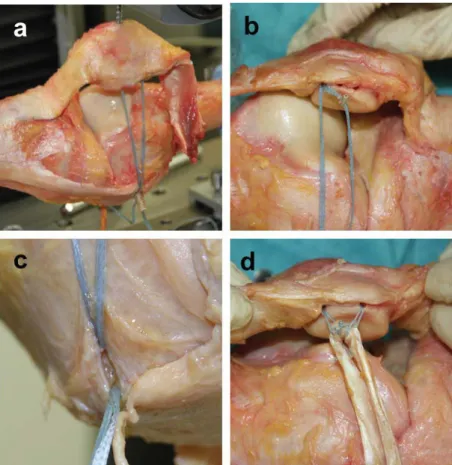
All native MPFL failed at the femoral insertion side. In group A, 5 specimens failed via pullout of the 4.75-mm knotless anchor at the femoral side (Figure 5-a), 3 specimens via pullout of the 3.5-mm knotless anchor at the patella side (Figure 5-b) and 1 specimen via fracture (cheese cut) of the femur without breakage of the knotless anchor (Figure 5-c). In group B, all specimens failed via pullout of the soft anchors at the patella side (Figure 5-d). There were no ruptures of the FT or ST.
Discussion
MPFL reconstruction using FT with knotless anchors was stronger than the
native MPFL and MPFL reconstruction using a ST with soft anchors at time zero. The current results showed this procedure obtained enough strength for MPFL reconstruction while avoiding complications associated with graft harvesting.
The gold standard of the autologous tendon graft was a hamstring tendon.
However, with autologous tendon harvest, there were risks to the donor site such as pain, hematoma, neurovascular damage, and infection (16). To avoid such risks, the MPFL reconstructions using various synthetic materials were reported (6) (12). Nomura et al.
(6) found favorable midterm follow-up outcomes of MPFL reconstruction using a Leeds- Keio artificial ligament. Using the Crosby and Insall grading system (17), they found only one knee of poor quality, while the remaining 29 were assessed as either good or excellent (6). However, their surgical fixation technique used a staple which led to significant levels of post-operative pain at the staple site (6). Recently, Lee et al. (12) reported clinical outcomes at 12, 24 and 48 months after surgery. In their study, there was a significant improvement between all preoperative and post-operative scores and no recurrences of patellar instability or dislocation noted in any patients during the follow-up period (12).
The mode of failure is important in order to understand the mechanical properties of the MPFL and the reconstructed MPFL. In this study, all native MPFL failed at the femoral insertion side, which agrees with clinical observation (18). Therefore, we believe
that our testing procedure might replicate the clinical injury situation. All reconstructed MPFL failed at the fixation site, regardless of graft materials. Since the tensile strength of the FT (937 ± 93 N) (13)and the ST (1060 ± 227 N) (19)is much higher than the strength of the native MPFL, initial fixation technique is very important.FT is a modern synthetic material made from an ultra-high molecular weight polyethylene with a braided jacket of polyester tape. Unlike autologous tendon graft, FT is less likely to stretch over time. Therefore, if sufficient graft fixation strength was obtained, it seemed that reliable stability could be maintained for a long term.
Multiple methods for graft fixation to the patella have been reported. Some surgeons preferred to use a bone tunnel technique to fix the graft, with others preferring to use a bone groove technique, suture anchor technique, and so on. Regarding the tensile strength of fixation techniques, Mountney et al. (20)reported that tensile strengths of three techniques, suture repair alone (37 N), suture anchors plus sutures technique (142 N) and blind-tunnel tendon graft reconstruction (126 N), were significantly lower than that of native MPFL (208 N). In addition, Criscenti et al. (15)reported that the tensile strength of native MPFL was 145 N. In our study, FT with knotless anchors (178.4 ± 4.4 N) provided sufficient ultimate load for MPFL reconstruction.
There were several limitations of this study. Firstly, we performed two different
surgical procedures on each specimen and fixation sites on the second reconstruction were 5-10 mm from the previous sites. There have been some anatomical studies for attachment of MPFL on the patella side (14, 21, 22, 23), and those reports demonstrated different results. Although there might be variation in the attachment of MPFL especially on the patella side, our surgical procedure in this study were not necessarily anatomic reconstruction. In addition, in this study, only the patella and femur were fixed to the material testing machine and the same part of the patella was pulled in the same direction in both MPFL reconstructions. The 5-10mm change in two fixation sites of the patella and one fixation site of the femur might have influenced the biomechanical results, because it could have led to differences in the direction of pulling force and reconstructed MPFL between the first and second reconstruction in the biomechanical setting of this study. Secondly, there was a small number of specimens with a relatively older than the patients who are indicated for MPFL reconstruction in clinical situations, because it is difficult to obtain fresh cadaver knees in our country and we were able to use only amputated knees which were donated for research. Thirdly, the current study demonstrated the biomechanical strength at only time zero. Any subsequent healing could not be considered, which would be an important factor for the ST autograft. Another limitation was that we compared two surgical procedures including four variables that
were FT with knotless anchors and ST with soft anchors. Because there was a limit to the number of specimens we could use in this study, a comparison was made between the surgical procedure we used before in our institution and the new surgical procedure.
Conclusions
The results of the current study demonstrated that FT with knotless anchor fixation was stronger than the ST with soft anchors fixation for MPFL reconstruction at time zero.
References
1. Bicos J, Fulkerson JP, Amis A. Current concepts review: the medial patellofemoral ligament. Am J Sports Med. 2007 Mar;35(3):484-92. PubMed PMID: 17303819.
2. Buchner M, Baudendistel B, Sabo D, Schmitt H. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005 Mar;15(2):62-6. PubMed PMID: 15782048.
3. Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res. 2007 Feb;455:93-101. PubMed PMID: 17279039.
4. Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008 Dec;90(12):2751-62. PubMed: PMID 19047722.
5. Maenpaa H, Lehto MU. Patellar dislocation. The long-term results of nonoperative
management in 100 patients. Am J Sports Med. 1997 Mar-Apr;25(2):213-7.
PubMed: PMID 9079176.
6. Nomura E, Horiuchi Y, Kihara M. A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar disklocation. Knee. 2000 Dec 1;7(4):211–5. PubMed: PMID 11104912.
.7. Deie M, Ochi M, Sumen Y, Adachi N, Kobayashi K, Yasumoto M. A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2005 Oct;13(7):522-8. PubMed: PMID 15968532.
8. Dopirak R, Adamany D, Bickel B, Steensen R. Reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft: a case series. Orthopedics.
2008 Mar;31(3):217. PubMed: PMID 19292257.
9. Schottle P, Schmeling A, Romero J, Weiler A. Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2009 Mar;129(3):305-9. PubMed: PMID 18704468.
10. Sillanpaa PJ, Maenpaa HM, Mattila VM, Visuri T, Pihlajamaki H. A mini-invasive adductor magnus tendon transfer technique for medial patellofemoral ligament reconstruction: a technical note. Knee Surg Sports Traumatol Arthrosc. 2009
May;17(5):508-12. PubMed: PMID 19165466.
11. Makovicka JL, Hartigan DE, Patel KA, Tummala SV, Chhabra A. Medial Patellofemoral Ligament Reconstruction Using All-Soft Suture Anchors for Patellar Fixation. Arthrosc Tech. 2018 Feb 12;7(3):e231-7. PubMed: PMID 29881694.
12. Lee PYF, Golding D, Rozewicz S, Chandratreya A. Modern synthetic material is a safe and effective alternative for medial patellofemoral ligament reconstruction.
Knee Surg Sports Traumatol Arthrosc. 2018 Sep;26(9):2716-21 PubMed: PMID 28929187.
13. Bisson LJ, Manohar LM. A biomechanical comparison of the pullout strength of No.
2 FiberWire suture and 2-mm FiberWire tape in bovine rotator cuff tendons.
Arthroscopy. 2010 Nov;26(11):1463-8. PubMed: PMID 20920836.
14. Nomura E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005 Oct;13(7):510-5. PubMed: PMID 15895206.
15. Criscenti G, De Maria C, Sebastiani E, Tei M, Placella G, Speziali A, Vozzi G, Cerulli G. Reconstruction of medial patello-femoral ligament: Comparison of two surgical techniques. J Mech Behav Biomed Mater. 2016 Jun;59:272-8. PubMed:
PMID 26894660.
16. Shah JN, Howard JS, Flanigan DC, Brpphy RH, Carey JL, Lattermann C. A Systematic Review of Complications and Failures Associated With Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocation. Am J Sports Med. 2012 Aug;40(8):1916-23. PubMed: PMID 22679297.
17. Crosby EB, Insall J. Recurrent dislocation of the patella. Relation of treatment to osteoarthritis. J Bone Joint Surg Am. 1976 Jan;58(1):9–13. PubMed: PMID 1249117.
18. Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations.
Knee. 2002 May;9(2):139-43. PubMed: PMID 11950578.
19. Hamner DL, Brown CH, Jr., Steiner ME, Hecker AT, Hayes WC. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999 Apr;81(4):549-57. PubMed: PMID 10225801.
20. Mountney J, Senavongse W, Amis AA, Thomas NP. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005 Jan;87(1):36-40. PubMed: PMID 15686235.
21. Conlan T, Garth WP, Jr., Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993 May;75(5):682-
93. PubMed: PMID 8501083.
22. Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2006 Jan;14(1):7-12. PubMed: PMID 16001289.
23. Mochizuki T, Nimura A, Tateishi T, Yamaguchi K, Muneta T, Akita K. Anatomic study of the attachment of the medial patellofemoral ligament and its characteristic relationships to the vastus intermedius. Knee Surg Sports Traumatol Arthrosc. 2013 Feb;21(2):305-10. PubMed: PMID 22491706.
Figure Legends
Figure 1. Specimen preparation and setting on a material testing machine
The proximal part of the femur (F) was placed horizontally in a custom-made apparatus on a material testing machine. The cancellous screw inserted into the patella was firmly gripped by a clamp on the crosshead. (P): patella
Figure 2. MPFL reconstruction
a. FiberTape was fixed by with knotless anchors at the patella and femoral side in Group A, b. Semitendinosus autograft was fixed by two soft anchors at patella, and fixed by an interference screw at the femoral side in Group B.
Figure 3. Ultimate loads of native MPFL and reconstructed MPFL
Mean ultimate load of group A is significantly higher than native MPFL and group B.
Error bars represent standard deviation. *, p < 0.05.
Figure 4. Stiffness of native MPFL and reconstructed MPFL
Mean stiffness of group A is significantly higher than native MPFL and group B.
Error bars represent standard deviation. *; p < 0.05.
Figure 5. Mode of failure
In group A, 5 specimens failed via knotless anchor pullout at the femoral side (a), 3 specimens failed via knotless anchors pullout at the patella side (b), and 1 specimen failed via fracture (cheese cut) of femur without breakage of knotless anchor (c). In group B, all specimens failed via soft anchors pullout at the patella side (d).
Figures
Figure 1. Specimen preparation and setting on a material testing machine
Figure 2. MPFL reconstruction
Figure 3. Ultimate loads of native MPFL and reconstructed MPFL
Figure 4. Stiffness of native MPFL and reconstructed MPFL
Figure 5. Mode of failure