Impact of a Concomitant Relaxation Technique Intervention
on M edical and Health Behaviors in Patients Treated
for Type 2 Diabetes M ellitus
Yuko Katada,
Kikuyo Koitabashi,
Syoichi Tomono
and Michiyo Oka
Background & Aims: The aim of the present study was to verify the impact of progressive muscle relaxation (PMR) in combination with breathing technique (breathing PMR) on self-control for stress management in patients undergoing treatment for type 2 diabetes mellitus. M ethods: Twenty-four patients participated and were followed during a 2-month pre-intervention (baseline) period and a 6-month intervention period. Changes in salivary amylase concentration, blood pressure, heart rate, HbA1c level,and objective indices including relaxation scales,coping behavior scales,and mental health patterns extracted from semi-structured interviews were assessed before and after the interventions. Results: There were significant differences in the physical indices(salivary amylase concentration,blood pressure,heart rate)and relaxation scales between the pre-intervention and post-intervention periods(p< 0.05-0.01). The HbA1c levels during intervention were stable in a better range compared with those of previous year (p<0.05-0.01). Subjective indices including coping behavior scales, mental health pat-terns, and other complaints tended to improve during concomitant breathing PMR. Conclusions: Continuous breathing PMR during treatment for type 2 diabetes mellitus may improve self-control and stress management.(Kitakanto Med J 2014;64:135∼148)
Key words: type 2 diabetes, breathing PMR, continued intervention, stress management, self-control
Introduction
According to the International Diabetes Federa-tion, type 2 diabetes mellitus is a lifestyle-related disease in which genetic factors and living habits are closely linked. It is increasing rapidly in countries around the world and accounts for 90% of all diabetes in Japan. The Annual Statistical Report of National Health Conditions published by the Health and Welfare Statistics Association of Japan lists disruption of lifestyle and various stressors, which are related to type 2 diabetes mellitus, as factors affecting health. Diabetes is a disease that requires regularity of lifestyle patterns and self-control, and patient education has been conducted to help individuals control symp-toms. It has also become important, therefore, for
type 2 diabetes patients to control stress, especially if their own insulin secretion is still maintained. One study on stress management in diabetic patients report-ed that effects were seen on tension and anxiety after 1-month use of a biofeedback method with progressive muscle relaxation (PMR). However, the extent to which stress was actually controlled and whether there was an effect in controlling actual blood glucose levels are not clear. Lane conducted an education interven-tion study with blood glucose as an outcome indicator and showed no clear effect on blood glucose control. Tokuda reported the effects with intervention periods of 1-3 months based on interviews,but thought that it would be necessary to look at the effects of longer term interventions in order to see improvements in living habits and modification of behavior.
Kitakanto Med J 2014;64:135∼148
1 Gunma University Graduate School of Health Sciences,3-39-22 Showa-machi,Maebashi,Gunma 371-8514,Japan 2 Formerly, Gunma University Graduate School of Health Sciences, 3-39-22 Showa-machi, Maebashi, Gunma 371-8514, Japan
Received : November 28, 2013 Accepted : March 13, 2014
Address: YUKO KATADA Gunma University Graduate School of Health Sciences, 3-39-22 Showa-machi, Maebashi, Gunma 371-8514, Japan
Research aims and significance
The purpose of this study was to show the effects of intervention with PMR in combination with a breathing technique (breathing PMR) as a means of stress management to raise the self-control ability of type 2 diabetes mellitus patients based on physiologi-cal and subjective indicators. Through this study,the effectiveness of breathing PMR as a means of stress management in type 2 diabetes mellitus patients could be examined, and at the same time, suggestions for instruction in the process through which patients con-tinuously implement relaxation techniques and improve their self-control ability could be obtained.
Patients and M ethods
1.Research design
This was a causal hypothesis testing study that used pre and post tests in one group, with an estab-lished baseline period and pre-intervention and inter-vention year about HbA1c.
2.Participants
The participants were male and female type 2 diabetes mellitus patients ranging in age from 20 to less than 75 years. All participants were being treated with oral medications only as outpatients at a large hospital that served as a regional base hospital. The participants had difficulty controlling their blood glucose levels, with HbA1c>6.5%. The selected patients were patients who were referred by their primary physician,who approved of the purpose of the study. The participants informed consent was
obtained after the purpose of the study had been explained.
3.Data collection period
Data were collected from May 2010 to April 2011.
4.Conceptual framework (Fig.1)
I made a conceptual framework using Mind-body Connection Theory and Homeostasis Theory. Breath-ing PMR reduces the stress response and promotes the relaxation response.
The stress reaction is reduced, and a relaxation reaction is promoted by breathing PMR. Relaxation reactions, such as pleasantness and a calm feeling, eliminate superfluous stimulation of the hypothalamus and pituitary gland, decrease sympathetic nervous tone, and reduce the blood sugar level. As a result, the blood sugar level in peripheral vessels is controlled to the proper level. This is because people return to the normal internal environment by the constant maintenance function of the body when stress is released. That is, by promoting homeostasis, the blood sugar level returns to normal. The relaxation method is used to regain the usual state of this internal environment (in this case, the blood sugar level).
5.Operational definition of terms
1) Progressive muscle relaxation with a breathing technique (breathing PMR): A method in which the relaxation response is deepened while a 9-muscle group is repeatedly tensed and relaxed in time with abdomi-nal breathing, in which long breaths are used with a ratio of inspiration to expiration of 1: 2.
Fig.1 Conceptual framework -The recovery model of the constant maintenance mechanism by generating and breathing PMR of the vicious circle by 2 type diabetics stress cognition
2) Relaxation response: A response in which the parasympathetic nerves come to predominate as a result of inhibition of the sympathetic nerves from performing muscle relaxation exercises with a breath-ing technique. Blood pressure and pulse rate stabi-lize,and secretion of stress hormones decreases. Sub-jectively as well, a sense of relaxation is felt, and positive experiences increase in this response.
3) Stress response: The sympathetic nerves are activated when experiences in daily life are taken as stress, and increases in blood pressure and pulse rate are produced. In the endocrine system, the cortisol level increases, and a hyperglycemic state is produced. In this response,subjectively negative experiences also increase as a cognitive response.
4) Experience: The sensation produced in patients by breathing PMR.
5) Stress management : Assistance provided by nurses to help patients establish the relaxation tech-nique in their daily lives and stabilize blood glucose levels.
6) Self-control: Regulation of stress by patients themselves.
6.Intervention method (Breathing PMR method)
The relaxation method with the gradual muscular flaccidity method added to the breathing method, which can increase parasympathetic nerve activity most simply,was adopted as a concrete technique. Using the technique developed by Jacobson the method of stress management to reduce advanced stress is carried out, and it continues to be widely used today. Furthermore,by repeated relaxation,normalization of blood sugar should occur, and the disease itself may then be controlled.
(Intervention time and month)
This is outpatient instruction given a total of seven times, once at the start of the intervention and then once a month for 6 months.
(Place)
Experimental measurements were made in a pri-vate examination room in the hospital outpatient clinic. To ensure quietness and privacy,a space large enough for the techniques to be practiced together with researchers was used.
(Breathing PMR method)
At first, both eyelids are closed, and then the patient grows calm while repeating the breathing tech-nique for about 1 min. Next,a group of nine muscles is tensed (both arms→ both legs→ both thighs→ gluteal region → chest→ both shoulders→ forehead → glabella and interior of the eyes→ jaw and lips) (about 5 sec)and relaxed (15-20 sec)in order
repeated-ly. While doing this,the muscles are felt to relax,and subjects confirm the sensation when they are complete-ly relaxed. This procedure is repeated for 20 min, while repeating the breathing technique again at the end of the procedure.
7.M easurement indicators and instruments 1) Physiological indicators
(1) Salivary amylase values
Salivary amylase is considered to be a stress marker secreted by the action of sympathetic nerves. It was used to confirm the changes in the stress level because it responds sensitively to stressors in several minutes; it was measured before and after the relaxa-tion technique was performed for a total of eight times in the baseline and intervention periods to provide feedback for the technique. Measurements were made using a salivary amylase type sympathetic nerve moni-tor (Cocoro Meter, Nipro Corp., Tokyo, Japan). Comparisons were made with the absolute values of the before and after measurements rather than with reference values.
(2) Systolic blood pressure and pulse rate
As indirect markers of autonomic nervous system activity, systolic blood pressure and pulse rate were measured a total of eight times,at baseline and once a month before and after implementation of the breath-ing PMR relaxation technique durbreath-ing the intervention period. This was done to monitor the subjects gen-eral status,with systolic blood pressure and pulse rate as markers of the relaxation response. Measurements were made on the same side using an automated sphygmomanometer (HEM-705IT, Omron Corp., Tokyo, Japan)
(3) HbA1c values
To monitor blood glucose control status,informa-tion on changes in HbA1c values from the baseline period through the intervention period was obtained from subjects medical charts a total of eight times, once a month during the interviews. Data from the same period of the previous year were checked using medical records to determine the seasonal fluctuation. According to the revised Diagnostic Criteria of Diabetes Mellitus (2010), HbA1c 6.5% indicates a chronic hyperglycemic condition. Since HbA1c is thought to reflect the glycemic condition for the past 1 -2 months,it was suitable as an indicator showing the fluctuations during the intervention period.
2) Subjective markers (1) Relaxation scale
The relaxation scale is a scale to measure the degree of change in the psychosomatic state with the relaxation technique, prepared with reference to the Stress Management Kit. It was used a total of seven
times, once a month before and after implementation of the breathing PMR relaxation technique,to evaluate the stress response. A high score indicates more relax-ation.
(2) Effective or negative spiral coping behaviors scale
The Active, effective coping behavior scale and passive, negative spiral coping behaviors scale devel-oped by Munakata was used to observe the state of stress over time in diabetic patients, starting before intervention. This scale consists of 16 items overall. Nine items showing stress are evaluated on a 4-step scale, with higher scores indicating worse stress. Seven items on stress elimination methods are evaluat-ed in 3 steps, with higher scores showing better stress elimination. Measurements were made at the end of the baseline period,after 3 months,and after 6 months. (3) M ental health pattern diagnostic test (M HP-1) A mental health diagnostic test developed by Hashimoto et al. was used to evaluate the response to events in daily life and mental health. It consists of 40 items in six subscales to measure stress (stress check list, SCL) and two subscales to measure level of pur-pose in life (quality of life, QOL). Four mental health patterns were determined using the SCL score (30-120) and QOL (10-40): the stress maladaptation type, the stress resistant type, the stress semiadapted type, and the stress adapted type. A high SCL score and a low QOL score indicate stress maladaptation.
(4) Introspection report at time of instruction To confirm the patients status at the time of breathing PMR instruction each month,subjects spoke freely of their experiences, and their statements were recorded.
(5) Record of practice in the home
During the intervention period, subjects were asked to freely record their reactions and opinions when practicing at home to confirm how well they had mastered the technique. The content of these records was checked during outpatient visits at the time of monthly instruction. Responses were given to ques-tions on practice,and at the same time,encouragement was given to continue practicing.
(6) Interviews at the ends of the baseline and inter-vention periods
Semi-structured interviews focusing on diabetes control and breathing PMR were conducted using an interview guide once each for 15-30 min at the end of the baseline period and at the end of the intervention period. The interviews were recorded. Changes experienced over 6 months of stress management with breathing PMR were reported as self-evaluations of self-control.
8.Experimental schedule (Fig. 2)
1) Baseline period (2 months) and intervention period (6 months): Because of circadian changes in physiological indicators, the same time of
ing)was used. Interviews,relaxation instruction,and all data measurements were done by a single researcher.
2) Check of self-learning records
Besides instruction by outpatient, about 20 min-utes,it taught at the house every morning and evening so that repetition self-practice might be carried out for six months. Self-practice at a house had experience recorded and I got it to report at the time of instruction of the relaxation at the time of outpatient consultation. In order to make self-practice at a house easy to perform, CD gradual muscular flaccidity method of Gunma University attached hospital relaxation out-patient creation was lent out.
3) Interviews at the ends of the baseline and interven-tion periods
9 .Sample size
The sample size calculation for a single-case design with an αlevel of 0.05 and a power of 80% with plans to use the Kaplan-Meier method yielded a total of 49 cases,with 25 in the control group and 25 in the intervention group.
Analytical techniques
1.Analysis of physiological indicators and scales Multivariate analysis of variance was done for items that could not be confirmed to have a normal distribution. When a normal distribution was con-firmed, a paired t-test with Bonferroni correction was used to compare with baseline, and the Wilcoxon signed rank test was used to compare before and after implementation of the relaxation technique. The t-test was used to compare the vicious circle coping behavior measure and the MHP-1,which is related to relaxation, before and after implementation of the relaxation technique. Data were analyzed using PASW Statistics version 18.0 (SPSS, IBM Company, Tokyo, Japan).
2.Analysis of interview transcripts
Berelson s content analysis method was used. Verbatim transcripts were made from the recorded
tapes. While being careful not to change the semantic content of recorded units,the content was expressed in single sentences,and units were classified by similarity of meaning. Content was abstracted and coded. Content signified by the code was further classified by similarity to make subcategories. The level of abstrac-tion for classified subcategories was raised to create categories. To increase the reliability and validity of the analysis results, findings were also examined by multiple researchers with experience in studies of relax-ation methods or in nursing practice. Cases in which there were multiple occurrences of two experiences in the context were divided and handled as multiple recorded units.
Ethical considerations
Before the study was begun, it was reviewed and approved by the Clinical Ethics Committee of the participating institution (Approval No.10-3).
Results
1.Characteristics of participants (Table 1) Requests to participate in the study were made to 27 patients,26 of whom performed breathing PMR for 3 months, and 24 of whom continued to perform breathing PMR for 6 months. One participant dropped out. To elucidate the effect of ongoing breathing PMR, the 24 patients who were able to continue for 6 months were the subjects of the analysis. They included 13 men and 11 women,with a mean age of 62.2±5.8 years (range 32-74 years). The mean duration of disease was 7.7±3.8 years. There were no differences by baseline age in both men and women, physiological indices, subjective scale scores, and age. As for the continuation of practice guidance,all partic-ipants received outpatient treatment and interview guidance with a researcher each time,once a month for 6 months. The mean number of practices at home was 39 (minimum 20,maximum 51),and nearly all partici-pants practiced once or more per day. Oral drugs used were Euglucon, Actos, Amaryl etc. After the intervention, drug dosages were reduced in two
sub-Table 1 Characteristics of participants (n=24)
Characteristics n % mean (SD) Age (years) 62.20 (5.81) Disease years 7.70 (3.83) Sex Male 13 54.2 Female 11 45.8
Oral drugs Euglucon
Actos one person decreases at the biginning
Amaryl one person decreases at the biginning
jects and remained the same in all others. In one patient,oral drug use decreased during the intervention period as compared to the previous year,but the other patients showed no changes. There was no large change in weight and amount of physical activity based on the interviews.
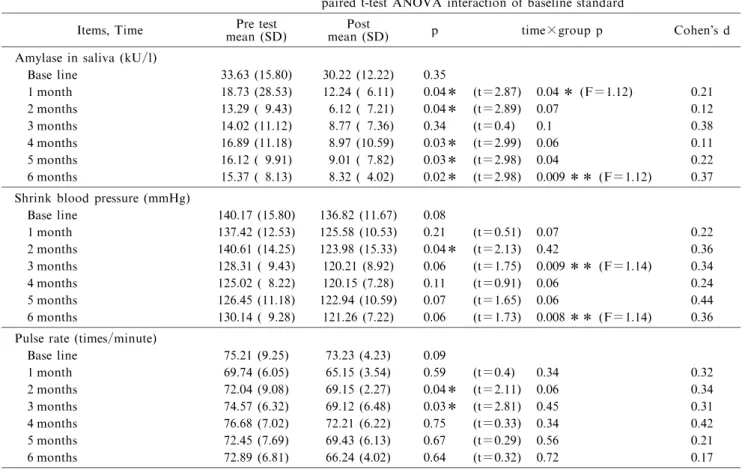
2.Physiological response (Table 2-1) 1) Salivary amylase value (kU/l)
Salivary amylase decreased significantly in com-parison paired t-test before and after enforcement, it fell intentionally from one month after (t=2.87, p= 0.04) to six months after (t=2.98, p=0.02) except for the three-month back (t=0.4, p=0.34) (p<0.05). By
the ANOVA analysis of variance of change of terms month,on month after an intervention term(F(1.12)= 5.675, p=0.04) is interactions. And the six-month back (F(1.12)=4.99, p=0.009) fell intentionally main effects to the baseline term.
2) Shrink blood pressure (mmHg) and pulse rate (beat/min)
Shrink blood pressure was by comparison paired t-test before and after enforcement, the two-month back (t=2.13, P=0.04) of the intervention term fell intentionally (p<0.05). By the ANOVA analysis of variance of change of term month,it fell intentionally interaction in of an intervention term three months(F (1.14)=5.12, p=0.009), and in six months to the
Table 2-1 Physiological indictors changes
paired t-test ANOVA interaction of baseline standard
Items, Time mean (SD)Pre test mean (SD)Post p time×group p Cohen s d Amylase in saliva (kU/l)
Base line 33.63 (15.80) 30.22 (12.22) 0.35 1 month 18.73 (28.53) 12.24 ( 6.11) 0.04* (t=2.87) 0.04* (F=1.12) 0.21 2 months 13.29 ( 9.43) 6.12 ( 7.21) 0.04* (t=2.89) 0.07 0.12 3 months 14.02 (11.12) 8.77 ( 7.36) 0.34 (t=0.4) 0.1 0.38 4 months 16.89 (11.18) 8.97 (10.59) 0.03* (t=2.99) 0.06 0.11 5 months 16.12 ( 9.91) 9.01 ( 7.82) 0.03* (t=2.98) 0.04 0.22 6 months 15.37 ( 8.13) 8.32 ( 4.02) 0.02* (t=2.98) 0.009 ** (F=1.12) 0.37 Shrink blood pressure (mmHg)
Base line 140.17 (15.80) 136.82 (11.67) 0.08 1 month 137.42 (12.53) 125.58 (10.53) 0.21 (t=0.51) 0.07 0.22 2 months 140.61 (14.25) 123.98 (15.33) 0.04* (t=2.13) 0.42 0.36 3 months 128.31 ( 9.43) 120.21 (8.92) 0.06 (t=1.75) 0.009 ** (F=1.14) 0.34 4 months 125.02 ( 8.22) 120.15 (7.28) 0.11 (t=0.91) 0.06 0.24 5 months 126.45 (11.18) 122.94 (10.59) 0.07 (t=1.65) 0.06 0.44 6 months 130.14 ( 9.28) 121.26 (7.22) 0.06 (t=1.73) 0.008** (F=1.14) 0.36 Pulse rate (times/minute)
Base line 75.21 (9.25) 73.23 (4.23) 0.09 1 month 69.74 (6.05) 65.15 (3.54) 0.59 (t=0.4) 0.34 0.32 2 months 72.04 (9.08) 69.15 (2.27) 0.04* (t=2.11) 0.06 0.34 3 months 74.57 (6.32) 69.12 (6.48) 0.03* (t=2.81) 0.45 0.31 4 months 76.68 (7.02) 72.21 (6.22) 0.75 (t=0.33) 0.34 0.42 5 months 72.45 (7.69) 69.43 (6.13) 0.67 (t=0.29) 0.56 0.21 6 months 72.89 (6.81) 66.24 (4.02) 0.64 (t=0.32) 0.72 0.17 * p<0.05 ** p<0.01 n=24 Table 2-2 Changes of HbA1c rate during experimental periods
paired t-test ANOVA interaction of baseline standard Items, Time intervention year
Non-mean (SD)
Intervention year
mean (SD) p time×group p Cohen s d
HbA1c (%) Base line 7.67 (1.19) 7.65 (1.34) 0.21 1 month (Oct.) 7.52 (1.32) 7.39 (1.20) 0.05 (t=0.41) 0.33 0.38 2 months (Nov.) 7.82 (1.97) 7.55 (1.27) 0.05 (t=0.42) 0.21 0.32 3 motnths (Dec.) 7.91 (1.25) 7.66 (1.33) 0.04* (t=2.71) 0.25 0.21 4 motnhs (Jan.) 7.72 (1.31) 7.53 (1.26) 0.04* (t=2.66) 0.11 0.37 5 months (Feb.) 7.32 (1.24) 7.56 (1.06) 0.07 (t=0.42) 0.22 0.33 6 months (Mar.) 7.55 (2.36) 7.45 (1.09) 0.05 (t=1.88) 0.72 0.42 * p<0.05 ** p<0.01 n=24
baseline term is main effects(F(1.14)=4.88,p=0.008). The pulse rate fell intentionally in two months (t=2.11, p=0.06) and three months (t=2.81, p=0.03) at comparison paired t-test before and after enforce-ment (p<0.05). There was no change with a signifi-cant intervention term to a baseline term at the ANOVA analysis of variance of change of term month.
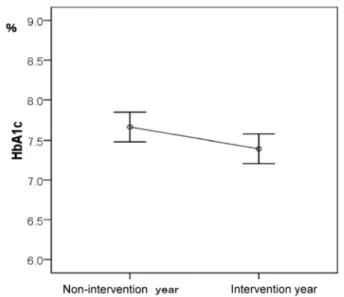
3) HbA1c values (%) (Table 2-2) (Fig. 3)
The HbA1c value was not getting worse through six months to the baseline term during the intervention six months after one month after an intervention term. It has been reported that the blood glucose level turns into a high price easily from December when change of the seasonal HbA1c value is especially pointed out, and it will hit at year ends and New Year holidays to February. Then, when the comparison with the period of the previous year was tried,the previous year was the direction of intervention year 7.39±1.20 and the previous year a high price in the significance level p<0.05 at multivariate analysis of variance in 7.67± 3.20.
3.Subjective responses (Table 3) 1) Relaxation scale
According to a paired t-test before and after the intervention, the relaxation scale, one of subjective responses, went up significantly (p<0.05, p<0.01) with intervention terms between one month (t=2.95, p=0.009)and six months(t=2.67,p=0.02),except for the intervention term of two months(t=1.81,p=0.06). 2) Effective or negative spiral coping behaviors
scale (Fig. 4)
At the end of the baseline period, 34.5% of sub-jects reported having stress related to physician s instructions or taking drugs for diabetes, and 21.3% reported stress related to family matters. No stress was reported related to getting along with people or the understanding of those around oneself. The most common stress elimination method (26.7%) was com-pensatory behavior consisting of eating something delicious, comfort eating, or drinking alcohol as a
reward when finishing work, although 6.5% adopted methods such as consulting with others. In per-sonal relationships, 11.3% reported being aggressive toward others when irritated even while reporting no stress that was related to getting along with people or the understanding of those around oneself. After 3 months, there was no stress related to visiting the hospital and living a regulated life, and among stress elimination methods,there was a decrease to 13.6% in comfort eating and drinking alcohol, while 0.4% responded that they were aggressive toward others. After 6 months, there was a decrease to 5.2% in the number of people with complaints related to physi-cian s instructions or taking drugs for diabetes, and slight increases from 2.3% to 5.6% in looking at things from a distance, 3.7% to 5.7% in having people understand my feelings of discomfort or anger, and 1.8% to 3.8% in trying to change my way of thinking and circumstances among stress elimination methods. However, there was no change over the 6 months in trying to create new prospects or plans (0.4%) and obtaining hints from people on solving problems.
Fig.3 HbA1c in the non-intervention year and the intervention year
Table 3 Relaxation scale, one of subjective responses
paired t-test ANOVA interaction pre
mean (SD) mean (SD)post p group p Cohen s dtime×
At the time of a start 17.88 (8.42) 16.43 (2.34) 0.46 0.42 0.43
Intervention term 1 month 16.71 (5.06) 27.54 (3.68) 0.009** (t=2.99) 0.04* 0.11 2 months 18.83 (5.65) 26.54 (3.40) 0.06 (t=1.81) 0.21 0.22 3 months 18.54 (5.71) 26.79 (3.46) 0.04* (t=2.01) 0.11 0.12 4 months 18.17 (5.42) 25.83 (3.89) 0.06 (t=2.45) 0.21 0.37 5 months 16.54 (3.93) 25.79 (3.59) 0.03* (t=2.59) 0.09 0.12 6 months 17.58 (3.82) 26.58 (4.44) 0.02* (t=2.67) 0.04* 0.11 * p<0.05 ** p<0.01 n=24
3) M HP-1 mental health scale (Fig. 5)
At baseline, the largest number (60%) was exhausted type (stress maladaptation type), after 1 month,the largest number(42.5%)was wheezing type (stress resistant type), and from 2-6 months,the largest number (mean 30.2%) was relaxed type (stress semiadapted type). The mean SCL score was 82 at the end of the baseline period and 50-69 after 1-6 months of intervention. The mean QOL score was 19 at the end of the baseline period and 21-24 after 1-6 months of intervention.
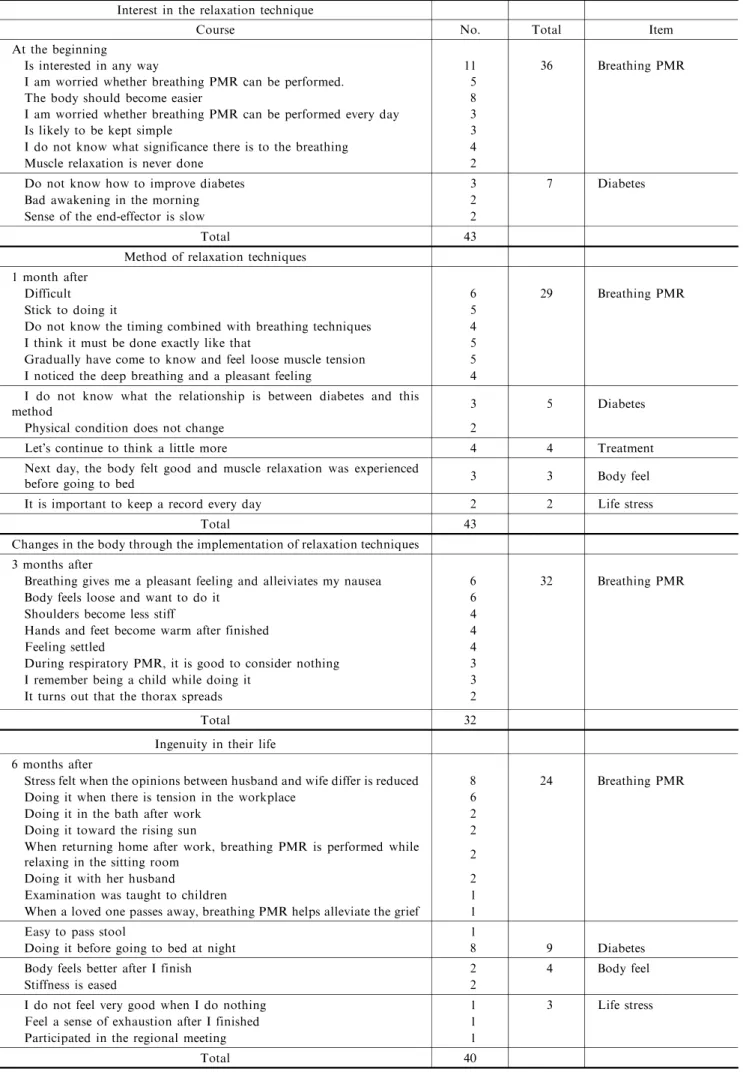
4) Introspection report
PMR status was followed every 3 months. Imme-diately after the start of the intervention, the largest number of statements(36)expressed interest in breath-ing PMR. After 1 month,the largest number of state-ments(29)was about how to perform breathing PMR. After 3 months, the largest number of statements (32) was about physical changes. After 6 months, the largest number of statements (24) was about areas where subjects themselves had made modifications in daily living.
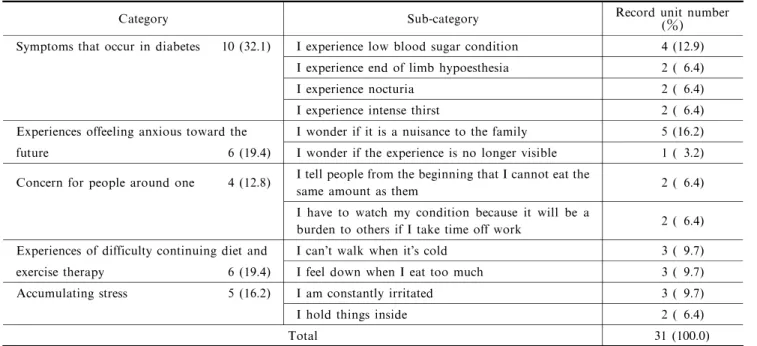
5) Content of interviews at the end of the baseline and intervention periods
Based on the results of content analysis of patients comments on self-control in diabetes, categories and subcategories were established (Tables 4-6). In the following, categories are shown in bold and sub-categories in italics. The results are explained using recorded units. [ ] are categories, and > are
subcategories.
(1) Content of experiences in everyday life at baseline period
Five categories and 12 subcategories were identified from the analysis, with 31 recorded units. The most common category was[Symptoms that occur in diabetes],accounting for 32.1% of all record-ed units. This category was relatrecord-ed to symptoms that were currently present due to diabetes, such as hypog-lycemia, cold sweats, and poor peripheral circulation, and symptoms that may, as far as the patient under-stands,occur in the future. The category of[Experi-ences of feeling anxious toward the future]described experiences that occur with progression of the disease stage, such as I think I may become a burden for my family>, and I am worried that I may lose my sight>. The category of[Concern for people around one] expresses patients concern for the people around them, such as I tell people from the beginning that I cannot eat the same amount as them>,and I have to watch my condition because it will be a burden to others if I take time off work>. The category of[Experiences of difficulty continuing diet and exercise therapy]ex-presses the difficulties patients have had in continuing their diet and exercise therapy, such as I can t walk when its cold>, and I feel down when I eat too much>. The category of[Accumulating stress]ex-presses the stress accumulated in patients during daily life,such as I am constantly irritated>, I hold things inside>.
Table 4 Participants subjective reports on breathing PMR Interest in the relaxation technique
Course No. Total Item
At the beginning
Is interested in any way 11 36 Breathing PMR
I am worried whether breathing PMR can be performed. 5
The body should become easier 8
I am worried whether breathing PMR can be performed every day 3
Is likely to be kept simple 3
I do not know what significance there is to the breathing 4
Muscle relaxation is never done 2
Do not know how to improve diabetes 3 7 Diabetes
Bad awakening in the morning 2
Sense of the end-effector is slow 2
Total 43
Method of relaxation techniques 1 month after
Difficult 6 29 Breathing PMR
Stick to doing it 5
Do not know the timing combined with breathing techniques 4 I think it must be done exactly like that 5 Gradually have come to know and feel loose muscle tension 5 I noticed the deep breathing and a pleasant feeling 4 I do not know what the relationship is between diabetes and this
method 3 5 Diabetes
Physical condition does not change 2
Lets continue to think a little more 4 4 Treatment
Next day, the body felt good and muscle relaxation was experienced
before going to bed 3 3 Body feel
It is important to keep a record every day 2 2 Life stress
Total 43
Changes in the body through the implementation of relaxation techniques 3 months after
Breathing gives me a pleasant feeling and alleiviates my nausea 6 32 Breathing PMR
Body feels loose and want to do it 6
Shoulders become less stiff 4
Hands and feet become warm after finished 4
Feeling settled 4
During respiratory PMR, it is good to consider nothing 3
I remember being a child while doing it 3
It turns out that the thorax spreads 2
Total 32
Ingenuity in their life 6 months after
Stress felt when the opinions between husband and wife differ is reduced 8 24 Breathing PMR Doing it when there is tension in the workplace 6
Doing it in the bath after work 2
Doing it toward the rising sun 2
When returning home after work, breathing PMR is performed while
relaxing in the sitting room 2
Doing it with her husband 2
Examination was taught to children 1
When a loved one passes away,breathing PMR helps alleviate the grief 1
Easy to pass stool 1
Doing it before going to bed at night 8 9 Diabetes
Body feels better after I finish 2 4 Body feel
Stiffness is eased 2
I do not feel very good when I do nothing 1 3 Life stress
Feel a sense of exhaustion after I finished 1
Participated in the regional meeting 1
Table 5 Content of experiences in everyday life at baseline
Category Sub-category Record unit number(%)
Symptoms that occur in diabetes 10 (32.1) I experience low blood sugar condition 4 (12.9) I experience end of limb hypoesthesia 2 ( 6.4)
I experience nocturia 2 ( 6.4)
I experience intense thirst 2 ( 6.4)
Experiences offeeling anxious toward the I wonder if it is a nuisance to the family 5 (16.2) future 6 (19.4) I wonder if the experience is no longer visible 1 ( 3.2) Concern for people around one 4 (12.8) I tell people from the beginning that I cannot eat the
same amount as them 2 ( 6.4)
I have to watch my condition because it will be a
burden to others if I take time off work 2 ( 6.4) Experiences of difficulty continuing diet and I can t walk when its cold 3 ( 9.7) exercise therapy 6 (19.4) I feel down when I eat too much 3 ( 9.7)
Accumulating stress 5 (16.2) I am constantly irritated 3 ( 9.7)
I hold things inside 2 ( 6.4)
Total 31 (100.0)
Record unit number (%) Table 6 Content of experiences in the everyday life at the end of the intervention period (6 months)
Category Sub-category Record unit number(%)
Becoming positive 22 (30.6) I experience cooling down 7 ( 9.7)
I can identify a short-term target that he can meet 8 (11.1)
I can have a familiar target 3 ( 4.2)
I can feel a change of pace 2 ( 2.8)
I feel you can recognize yourself 2 ( 2.8) Being able to cope with stress 12 (16.7) I am able to deflect negativity 4 ( 5.5) I improve blood pressure values 3 ( 4.2) I eliminate the burden of feelings 3 ( 4.2) I feel in touch with with reality 2 ( 2.8) A body feeling better 12 (16.7) I feel muscle tension slowly being released 8 (11.1) I moderate headache and stiff neck 2 ( 2.8)
I feel warm hands and feet 2 ( 2.8)
A feel to sleep effects 5 (6.9) I can fall asleep without using drugs 2 ( 2.8) I experience a sense of deep sleep 2 ( 2.8) I wake up feeling better in the morning 1 ( 1.3) Distancing oneself from stress in daily life
5 (6.9)
I feel that the problems of family care can be forgot
ten 2 ( 2.8)
-I can be interrupted to take care of children 1 ( 1.3)
I relieve tension from work 2 ( 2.8)
Looking back on oneself 6 (8.4) Maintain my own pace now 3 ( 4.2) I am able to think calmly about things 3 ( 4.2) Being able to regulate appetite 8 (11.1) Eat too much and feel down less often 3 ( 4.2)
Become calm by performing breathing PMR before
meals 4 ( 5.5)
I can tell people about dietary restrictions due to
diabetes 1 ( 1.3)
Difficulties learning the technique 2 (2.8) I feel performing correct breathing PMR from the
beginning 1 ( 1.4)
I feel doing it only as shown 1 ( 1.4)
Total 72 (100.0)
(2) Content of experiences in everyday life at the end of the intervention period after 6 months Based on the analysis, 8 categories and 25 sub-categories were identified, consisting of 72 recorded units. The category of[Becoming positive]was the most common,with 30.6% of all recorded units. This was followed by[Being able to cope with stress]. [A body feeling better]and[A feel to sleep effects]. The meanings of the category[Distancing oneself from stress in daily life]was being able to temporar-ily distance oneself from datemporar-ily stresses,such as nursing care for ones husband,looking after children,or stress from work for the category. [Looking back on one-self]meant being able to look steadily at oneself,such as Maintain my own pace now, and being able to think calmly about things>. The category of[Being able to regulate appetite]meant being able to control the foods one most enjoys(the control of foods is most difficult for diabetic patients), such as Eat too much and feel down less often>, and Become calm by performing breathing PMR before meals>,[Diffi-culties of method of breathing PM R],such as Every time thinking method in first time>, Thinking of standard method>
Discussion
1.Evaluation of acquisition of the relaxation method and use in daily life
Once the breathing PMR had been practiced, a general decrease was seen in systolic blood pressure after performing the technique, and a significant decrease was seen in the pulse rate after 1-2 months of intervention. Salivary amylase values showed that a relaxation response was generally obtained, with the exception of some data. Among subjective responses, the sense of relaxation rose significantly through the 6 months, suggesting that the relaxation technique with breathing PMR was acquired sufficiently. In addi-tion,it was seen from the practice records at home that the relaxation technique came to be adopted in normal daily life and was used appropriately in the several stressful situations each patient encountered in daily life. Use of the breathing PMR technique in daily life is thought to lessen the burden on the body from sustained, unnecessary tension and decrease the occur-rence of emotional instability. The stability of the physiological and subjective responses produced by relaxation also improved subjects ability to cope with stress in daily life and produced stability in daily events. These findings suggest that this technique is effective as a means of self-control.
2.Evaluation of self-control in diabetes (1) Evaluation of physiological responses
Based on the comparison with HbA1c values from the same period in the previous year (7.52%± 1.32%-7.91%±1.25%),the data from the intervention year (7.39%±1.21%-7.66%±1.33%) were significant-ly more stable,and there was no instability or increase in blood glucose levels during the winter months, to which diabetics are thought to be susceptible. If it thinks from there not having been a change in how or weight and change of an oral medicine, it will be thought that the breathing PMR hand an effect in stabilization of the blood glucose level. An interven-tion term,for the 2 or 3 month,although it hit at the blood glucose aggravation time of the year ends and New Year Holidays it is supposed that are easy to happen to a diabetic, the instability of the blood glucose level or aggravation was not caused.
Wales thought that there were cases when vari-ous stresses in daily life increased the release of insulin resistance hormones and worsened glycemic control, and cases when insulin resistance relates to coping behaviors for stress, further worsening glycemic con-trol. The blood glucose stability in the present study was thought to have been a result of the relaxation response from implementation of the relaxation tech-nique in a stressed state,which stimulates hormones in the brain and acts in autonomic nervous system regula-tion. In addition, psychological stress invites emo-tional turbulence, decreases motivation for treatment of diabetes, and lowers compliance with treatment.
Moreover,in order that whether it is rapid change of the blood glucose level may advance hardening and aging of a blood vessel quickly, stabilization of the blood glucose level on the 1 in a diabetic is made into medical treatment and a nursing instruction item. That is m it can be said that stabilization of the blood glucose level important in complications. Diabetic patients on oral medications still have remaining endo-crine function of the pancreas, and the stability in blood glucose levels with the relaxation technique in the present study was also thought to be important in prognosis, considering the need for daily life manage-ment with diabetes over the long term. Marked hyper-glycemia is thought to occur from absolute insulin deficiency and excessive secretion of glucagon by mild adrenergic activation in times of stress in diabetics. In the present study, blood glucose levels were stable, blood pressure and pulse rate decreased, and salivary amylase levels decreased. This may have been due to the experience of relaxed feelings after breathing PMR, which is also supported by the significant rise in the relaxation score mentioned above, and emotional sta-bility.
One other issue is the process of bringing about a change in the coping behavior of self-control in diabet-ic patients by having them experience and acquire sufficient skill in the relaxation method in the medium and long terms. It is said that, in people with diabetes, control of blood glucose leads to higher QOL, but controlling blood glucose also becomes a source of stress. This makes continuation of diet and exercise therapy more difficult, producing a nega-tive spiral of higher blood glucose levels. Amidst this kind of dilemma,it becomes more difficult for individ-uals to accept diabetes and continue modified behav-iors. With consideration of the problems in conven-tional diabetes education raised by Kaneko, support for self-control in diabetic patients is thought to be important.
This study important effects that the patients in this study,who tended not to visit their doctor regular-ly,were able to participate in the program continuous-ly for 6 months may have been that guidance was conducted together with regular medical examinations. However, it is also thought that regular involvement with the instructor at the time of doctor visits sustained motivation for practice and enhanced the process of acquiring the technique. The things patients said in introspection reports at the time of instruction are things that lead to better patient support and help them recognize their experiences and face themselves.
Polosky stated that the sensation of comfort not only helps to stabilize brain hormones but may also lead to making repeatedly performed behaviors habit-ual. The present relaxation technique is thought to improve the psychosomatic correlation, produce a sensation of calm comfort,and promote the process of repeated practice so that the technique becomes habit-ual.
(2) Evaluation from subjective responses
From the MHP evaluation, the sense of satisfac-tion with life in the baseline period decreased depend-ing on the levels of stress and purpose in life. A change was seen over 6 months from a state of continu-ous stress and both mental and physical fatigue(wheez-ing type)to the ability to regulate mental and physical stress (relaxed type) by continuous intervention. The final MHP evaluation showed an increased number of subjects who needed to set specific targets for the future.
The stress peculiar to diabetic patients appeared in the stress appraisal conducted in the baseline period. Because of treatment other than for the general stress of job burdens and relationship and family problems, patients self-evaluations are affected by not being able to do the same things as people around them and the reactions of those people. Complications and anxiety
about hypoglycemia are also thought to exist. Another factor is the existence of unpleasant physical symptoms and decreased QOL. Diabetics are aware of diverse hypoglycemic symptoms. More than half experiences sweating and shaking of the hands, and nearly half is aware of hunger sensations, decreased concentration ability, and malaise. These symptoms cause deterioration in the quality, albeit temporarily, of daily activities, work, study, and personal relation-ships. Emotionally as well, symptoms of irritability, testiness, and sadness with crying are reported. It is thought that decreased motivation to engage in things and the effects on personal relationships may lead to decreased QOL. Considering this, stress content was surveyed by questionnaire from the baseline period until after the intervention. In the baseline period,in addition to anxiety about outpatient visits for diabetes and self-control,compensatory behaviors such as com-fort eating or harsh treatment of others decreased after 3 months of intervention. After 6 months,behavioral changes were seen, including distancing from some of those things or a change of situation. However, new prospects or attempting to make plans was not achieved,which is in agreement with the MHP results. With ongoing interventions in the future,it is thought that self-control can be achieved through effective stress management by setting targets suited to the indi-vidual patient and presenting specific, feasible plans. In the analysis of experiences after 6 months, subjects spoke of their experiences of having diabetes in addi-tion to their experiences of breathing PMR. Changes were seen from before intervention in the categories of [Experiences of restfulness], [Experiences of becoming more forward-looking], and[Experiences of regulating stress]. It was shown that the effects of excessive sympathetic nervous system activity can be lessened by regularly practicing the relaxation response. In addition, from the statement that my arms and legs become warm, it may be thought that blood flow is promoted by PMR with respect to peripheral vessel disorders from diabetes. Continu-ous support with a method that enables patients to make changes to their individual lives is important. Thus, it is thought that, together with patients own appraisal of stress, the range of relaxation techniques for self-control that are easy for patients to incorporate in their own lives is expanded for type 2 diabetes patients who have difficulty controlling blood glucose. In this study, patients spoke of their experiences that lead to stress,such as[Experiences of feeling anxiety toward the future]and[Experiences of symptoms], but after 6 months they did not speak of the negative stress coping methods for vague anxiety that they had used before intervention. It is thought that breathing
PMR had become one stress coping method in their lives.
(3) Suggestions obtained and proposals for the future
Based on the above,a breathing PMR intervention model for type 2 diabetes mellitus patients was devel-oped. In addition to individual factors,various stres-sors cause worsening of blood glucose control. How-ever, a state of self-control is reached, and blood glucose values stabilize through repeated practice of breathing PMR, which produces a chronic state in which the parasympathetic nervous system is domi-nant, together with the accumulation of subjective experiences. In 3 months,the blood sugar level stabil-ized, and although blood pressure and pulse rate fell, evaluations of the patients subjective reactions showed that the changes had not yet been fixed. This success heightens interest in the relaxation technique, which may lead to a positive cycle for a stable life. Continu-ous follow-up is needed to reach this cycle, in which the involvement of nurses is key.
Conclusion
Using a progressive muscle relaxation technique with breathing exercise in type 2 diabetes mellitus patients who had difficulty controlling blood glucose through outpatient treatment improved the patients status after intervention compared to the baseline period.
1.Acquisition of the relaxation technique
After practicing the technique, a relaxation response was obtained, and skill in the technique was acquired. Through continuing,repeated practice,the technique can also be matched to the lives of individ-uals for self-control of diabetes.
2.Control of diabetes
(1) HbA1c values did not have big changes for 6 months. However, the intervention year fell inten-tionally in comparison with the same time of the previous year.
(2) In the MHP mental health score, the stress maladaptation type was the most common at the end of the baseline period, the stress resistant type was the most common after 1 month of intervention, and the stress semiadapted type was the most common at 2-6 months of intervention.
(3) In the coping behaviors scale, compensatory behaviors of comfort eating and drinking alcohol were common for stress related to doctors instructions and taking medications at the end of the baseline period. After 6 months, however, these behaviors decreased, and more subjects performed specific stress elimination
techniques.
(4) In the interview at the end of the baseline period, subjects spoke of their experiences of having diabetes, while after 6 months, they spoke of their experiences related to self-control for diabetes.
Implementation of breathing PMR may increase parasympathetic nervous system activity and produce a state of relaxation, and it stabilizes blood glucose levels in patients with difficulty controlling blood glucose. In addition, it may also be a technique that does not have a large effect on systemic circulatory dynamics. This technique can be incorporated into daily life over the long term even in patients in whom glycemic control is difficult.
Study limitations and issues
A limitation of this study was the small number of patients,since it was a long-term intervention lasting 6 months. In the future,it will be necessary to conduct further studies with larger numbers of diabetic patients. To further clarify the long-term effects,there is a need for investigations of indications for programs that are altered to suit individual usage circumstances in daily life.
Acknowledgments
The authors would like to express their sincere appreciation to all the subjects who participated in this study,to the people at the hospital where the study was performed, and to everyone in their laboratory. The authors would also like to thank the physicians who cooperated to make this study more valuable. This study was supported by a 2009 research grant from the Gunma Health Foundation Research Promotion Pro-ject. Part of this study was presented at the 14th East Asian Forum of Nursing Scholars.
References
1. International Diabetes Federation. Oral health for people with diabetes 2009.
http://www.idf.org/webdata/docs/Japanese GMPG Final 280308.pdf
http://www.idf.org/webdata/docs/OralHealth EN RTP. pdf Accessed Dec. 22, 2012
2. The Annual Statistical Report of National Health Condi-tions. Health and Welfare Statistics Association of Japan 2011; 58: 1-499.
3. Kaneko E, Sakurakawa E, Watanabe K. Tonyobyo ni okeru stress to kango (The stress which can be set The stress of nursing from Diabetes).Rinshokango 2001; 26: 170-176 (in Japanese).
4. Oshita S, Hakoishi K, Knematu Y. 2gata tonyobyo kanja no stress to stress taisho kodo (2 type diabetes The theory of stress-coping behavior).Journal of Iwate Society of Nursing Science 2009 ; 3: 16-23 (in Japanese).
Selye ni tuite (Stress to the application Selye to a healthy design Attach and by the bio feedback method). Tokyo : Sogen-Igakushinnsho, 1980 (in Japanese).
6. Baldree KS,Muphy SP,Powers MJ. Stress indentification and coping patients on hemodialysis. Nursres 1982; 31(2) : 107-112.
7. Suga K. Tonyobyo eno biofeedback ni yoru relaxation kunren (Diabetes the relaxation training). Journal of Japanese Society of Nursing 2007; 34: 23-25(in Japanese). 8. Lane JD. Relaxation Training for NIDDM. Diabetes
Care 1993; 16: 1087-1094.
9. Tokuda K. Image kokyuho to kinshikanho ni yoru kibunhenka-Futatsu no giho no kyotsuten to soiten-(Image breathing method to depend by a muscular flaccidity method feeling change to depend -The common feature of two techniques To the mental healthy pattern of the valid-ity). Ritsumeikan-Ningenkagaku-Kenkyu 2008; 16: 1-12 (in Japanese).
10. Koitabashi K, Ohno N, Ohostuka T. Relaxation ni yoru suimin eno enjo nyuinchu no gan-kanja o taisho to shite (support for sleep by relaxation-cancer inpatients). Bulle-tin of Saitama College of Health 1995; 20: 81-89 (in Japanese).
11. Jacobson E. (Watanabe T. transl.) Businessman no relax kenkoho (Relaxation the healthy way) (1st ed). Tokyo : Yukishobou, 1963 (in Japanese).
12. Kondo Y. Gan-kanja ni taisuru zenshinteki-kinshikanho no keizoku-kainyu no koka ni kansuru kenkyu (effects of repeated intervention with progressive muscle relaxtion in cancer patients). Journal of Japanese Society of Cancer Nursing 2008; 22: 86-97 (in Japanese).
13. Yamaguchi M, Hanawa S, Yoshida H. Daeki amylase shiki kokanshinkei monitor no kisoteki seino (salivary amylase type sympathetic nerve monitor fundamental perfor-mance). Japanese Society for Medical and Biological Engineering 2007; 45: 161-168 (in Japanese).
14. Kobayashi S, Koitabashi K. Relaxation gairai ni okeru shiyo no shinraisei no kensho (relaxation visitors which can be set at a center is the reaction of the cognitive of the index of a difference). Journal of Japan Society of Nursing Research 2011; 34: 33-37 (in Japanese).
15. Munakata K. Saishin kodokagaku kara mita kenko to byoki (Newest behavioral science of the reliability). Tokyo : Mejikarufurendo-sha 1996; 16-29 (in Japanese). 16. Hashimoto N,Iwasaki K,Tokunaga M,et al. Daigakusei
no seishinteki kenkou pattern ni tuite. First Fukushi University Kiyo Sokan-go 2005; 1-12 (in Japanese). 17. Koitabashi K, Kondo Y, Yanagi N. Zennshiteki kin
shikan ho CD 2004 Merurinnchi.
18. Funashima N. Shituteki kenkyu eno chosen (Callenges of content analysis). Tokyo : Igaku-Shoin 2007; 2: 40-75 (in Japanese).
19. Kubo A. Tounyoubyou no stress management. Chiryo 1995; 77: 123-127 (in Japanese).
20. Benson H. (Nakano M, Kumano H, Kuboki T. transl.). Relaxation hanno (The relaxation response) (1st ed). Tokyo : Seiwa Shoten 2001 (in Japanese).
21. Koitabashi K. Zenshinteki-kinshikanho (Progressive mus-cle relaxation). In : Arakawa S, Koitabashi K(eds.). Kango ni ikasu relaxation-giho holistic approach (Relaxa-tion technique to make use of nurses holistic approach)(1st edn, pp.30-52). Tokyo : Igaku-Shoin 2001 (in Japanese). 22. Norris SL, Schmid CH, Lau J. Self-management
educa-tion for adults with type 2 diabetes a meta-analysis of the effect on glycemic control. Diabetes Care 2002; 25: 1159-1171.
23. Wales JK. Does psychological stress cause diabetes? Diabetic Medicine 1995; 12: 109-112.
24. Jones H, Edwards L, Vallis TM. Changes in diabetes self-care behaviors make a difference in glycemic control the Diabetes Stages of Change study. Diabetes Care 2003; 26: 732-737.
25. Faith SL, Jacqueline DJ. Sleep Quality and Quality of Life in Adults With Type 2 Diabetes. Diabetes Education 2011; 37 (3): 347-355.
26. Grauw WJ, Gerwen WH, Lisdonk EH. Outcomes of audit-enhanced monitoring of patients with type 2 diabetes. The Journal of Family Practice 2002; 51: 459-464. 27. Oka M. Kanja kyoiku ni tsukaeru hokenkodo
model-shiennaiyo no furikaeri ni yakudatsu client no hokenkodo sogosayo model(IMCHB)o chushin ni-(At a center interac-tion model/(IMCHB)/of the kuraimantle which is useful for health behavior model 2 assist content which can be used for 1 patient education to turn round/health behavior). Diabetes Care 2009 ; 6: 14-19 (in Japanese).
28. Robin RR, Peyrot M. Psychosocial problems and inter-ventions in diabetes: A review of the literature. Diabetes Care 1992; 15: 1640-1657.
29. Polosky WH, Jacobson AL, Arderson BJ, et al. Assess-ment of diabetes related distress. Diabetes Care 1995; 18: 754-760.
30. Nishi M, Okazaki K, Murata K. Teiketto shojo no tayousei to ketto ninshiki training no yukosei (Hypog-lycemic diversity, and blood glucose recognition training seen from the verification). Tonyobyo 2009 ; 52 (suppl. 1): s-133 (in Japanese).