IRUCAA@TDC : Application of resin-coating methods: effect of different bur grinding on micro-tensile bond strength to coated dentin
全文
(2) 2008 Graduation Thesis. Application of resin-coating methods: effect of different bur grinding on micro-tensile bond strength to coated dentin. by. Takumi Oishi. Promotors:. Professor Yoshito Hirai Assistant Professor Atsushi Kameyama. (Department of Operative Dentistry, Tokyo Dental College). 1.
(3) CONTENTS Introduction……………………………………………………………………………3 Chapter 1. Resin-dentin adhesion: A review of the literature 1.1. Restorative procedures for caries treatment……………..5 1.2. Background and classification of adhesive systems…….5 1.3. Clinical factors influencing resin-dentin bonding……..8 1.4. Influence of smear layer on dentin bonding……………10 1.5. Resin-coating method for indirect restorations…………11 1.6. References………………………………………………….11. Chapter 2. Influence of different bur grinding on micro-tensile bond strength in resin-coated dentin 2.0 Abstract……………………………………………………19 2.1. Introduction………………………………………………..19 2.2. Materials and methods…………………………………..20 2.3. Results…………………………………………………….23 2.4. Discussion………………………………………………...24 2.5. Conclusions……………………………………………….26 2.6. References………………………………………………..27. Chapter 3. General discussion and conclusions 3.1. Indirect vs. direct restorations: which is more reliable for 3.2. 3.3.. posterior teeth?............................................................33 General conclusion……………………………………34 References………………………………………………..34. Acknowledgments…………………………………………………………………36 Tables and Figures Appendix. 2.
(4) INTRODUCTION. Minimally invasive dentistry using adhesive material for direct restoration is one of the recent concepts in caries treatment. The development of restorative materials has made posterior restoration possible, but the effectiveness of this method depends on the bonding performance between the restorative material and the prepared cavity, and at the present time we can remove only the infected area and perform esthetic restoration. Despite such a limitation, in Japan, posterior restoration using metal inlay remains the first choice of treatment for molar caries. While restored metal has sufficient tolerance to occlusal force, it also has disadvantages in that it requires considerable tooth reduction and can cause esthetic defects. As an alternative method, indirect esthetic restoration using CAD/CAM technology is starting to prove popular. This thesis investigates how to restore posterior teeth using indirect restorative material in an attempt to develop a more reliable method for clinical application. In Chapter 1, I summarize the historical development of restorative procedures and review the literature on factors affecting clinical performance. In Chapter 2, I evaluate and discuss the influence of different bur grinding on bond strength, making comparisons between indirect restorative material and resin-coated dentin. And finally in Chapter 3, I first discuss how to choose the restorative method and material to use based on my investigative results and a review of the literature, and then discuss how to perform indirect restoration to achieve reliable and durable results.. 3.
(5) Chapter 1. Resin-dentin adhesion: A review of the literature. 4.
(6) Chapter 1 1.1.. Resin-dentin adhesion: A review of literature. Restorative procedures for caries treatment. The extent of cavity preparation for direct restoration with adhesive material is generally limited to removing only infected tooth tissue. Typically, the infected dentin area is stained with caries detector, then removed using rotary cutting instruments only within the stained dentin tissue (Fusayama 1996). The subsurface retained in the caries-affected but disinfected region is the so-called inner carious dentin. Since the dentin tubules in this area are filled with numerous whitlockite crystals, the demineralized tissue can remineralize itself. Immediately after caries removal, bonding is carried out in the prepared cavity and the cavity is filled with tooth-colored restorative material such as resin composite or glass-ionomer cement. The filled material is then hardened and the finishing/polishing procedure is performed. By contrast, the cavity preparation method for indirect restoration is based on five required factors (conditions) proposed by Black (1955): adequate form of cavity outline, sufficient retention form, sufficient resistant form, adequate marginal form, and convenient form if necessary. Even if the caries infection is partial, the cavity must be prepared to satisfy these factors. Therefore, considerable amounts of healthy tooth tissue must be removed. After cavity preparation, an impression of the prepared cavity is taken before the cavity is filled with temporary filling material. A restored inlay block is then prepared by a dental technician and cemented with luting material at the next appointment.. 1.2.. Background and classification of adhesive systems. 1.2.1. Pre-1980’s: The total-etch concept After the introduction of acryl-based resin and acid-etched enamel adhesion by Buonocore in 1955, several researchers attempted to adhere resin material to dentin. In 1979, Fusayama et al introduced a method of etching using 40% phosphoric acid gel entirely within the cavity, the so-called “total-etch concept”. This procedure which removes smeared debris that interferes with the. 5.
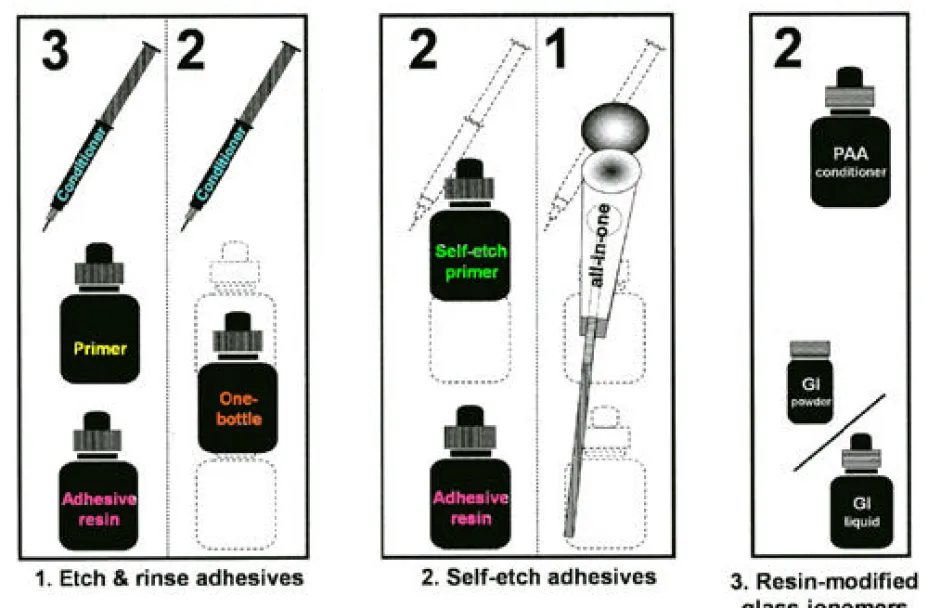
(7) penetration of acid etching material is surely necessary, but their attempts were unsuccessful because the phosphoric acid etching to dentin was too strong and the resin monomer did not penetrate into the demineralized and collapsed collagen network sufficiently. 1.2.2. Discovery of the hybrid layer In the early 1980s, bonding agents designed for etched dentin were developed. Clearfil Bond System-F (Kuraray Medical) contained 5% 2-mechacryloxymethyl phenyl phosphoric acid (Phenyl-P) and 30% 2-hydroxyethyl mechacrylate (HEMA). In 1981, Misu demonstrated that Clearfil Bond System-F (Kuraray Medical) created a film of membrane structure at the adhesive interface (Misu 1981), providing one of the first hints toward the eventual discovery of the ‘hybrid layer’ by Nakabayashi (1982). The hybrid layer is the structure formed by infiltration of the resin monomer into the smear-removed and partially demineralized dentin subsurface. However, as mentioned above, excess demineralization may cause insufficient infiltration, leading to a gap at the adhesive interface. Nakabayashi discovered the hybrid layer in 1982 when attempting dentin bonding between 4-META/MMA-TBB resin and dentin etched with 10% citric acid including 3% ferric chloride. This layer is a resin penetration zone of a few micrometers thickness. 1.2.3. 3-step etch & rinse adhesive systems In 1984, Munksgaard and Asmussen described a new bonding system based on complete removal of the smear layer with 0.5% EDTA followed by rinsing with water and application of primer composed of a mixture of 5% gluraraldehyde and 35% HEMA in water, known as Gluma. The three steps of etching, priming and bonding continue to make up the current mechanism of dentin bonding, although contemporary 3-step systems are composed of approximately 35% phosphoric acid gel as the etching agent in place of EDTA (Table 1-1, Fig. 1-1). 1.2.4. 2-step self-etch adhesive systems In the early 1990’s, Watanabe et al (1990, 1994b) introduced a novel primer. 6.
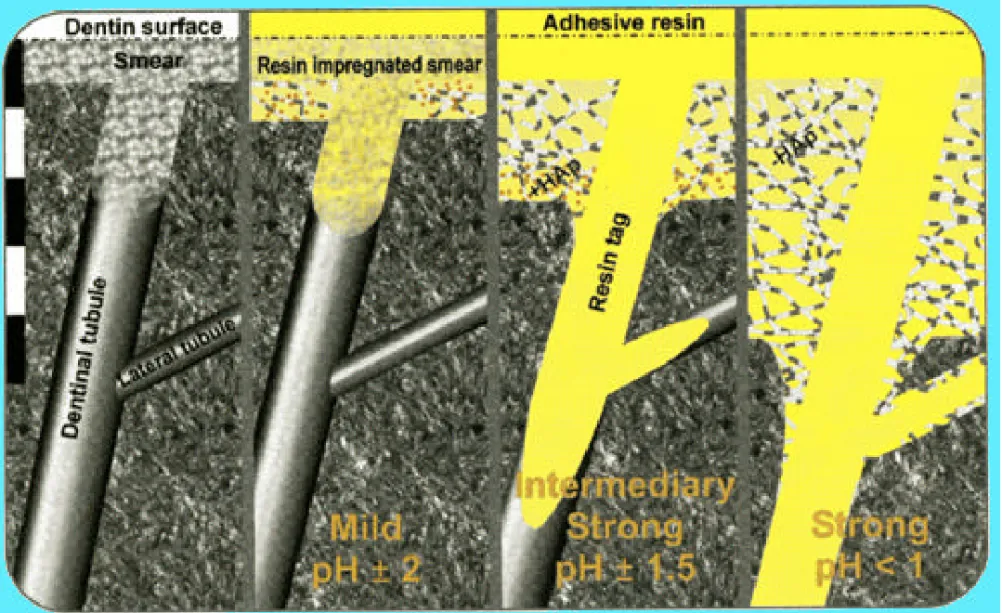
(8) having dual functions of etching and priming with an acidic monomer, which was commercially developed as Clearfil Liner Bond II (Kuraray Medical), a two-step self-etch adhesive. The main disadvantage of two-step self-etch adhesives is that they leave a residual smear layer. Since the acidity of self-etching primer is generally milder than acid etchant, the smear layer is not completely removed or hybridized with the adhesive resin (Nakabayashi and Saimi 1996). Some reports suggest a mechanical weakness of the hybridized smear layer between the adhesive and hybrid layers (Nakabayashi and Saimi 1996; Miyasaka and Nakabayashi 1999). 1.2.5. 2-step etch & rinse adhesive systems In 1992, Kanca introduced the unique method known as the “wet bonding technique” (Kanca 1992). After the phosphoric acid etching to dentin, the exposed collagen network is shrunk by strong air drying. The shrinkage of collagen interferes with the penetration of resin monomer into the demineralized region. Kanca therefore attempted the penetration of acetone-based primer/adhesive solution into the phosphoric acid-etched and water-rinsed dentin in a moist environment. Although this excellent idea created an effective technique, wet bonding is technique-sensitive in the clinical situation because it is difficult to produce a uniform wet state in all cases. Undesirable effects of over-drying or over-wetting have been reported (Tay 1996). 1.2.6. 1-step self-etch adhesive systems Single-step adhesive systems successfully bring together the three procedures of etching, priming and bonding into only one step. Theoretically, this means that the bonding resin solution can diffuse into the demineralized region reliably. However, in general, the dentin bond strengths of the one-step adhesive systems are reported to be lower than those of the multi-step systems. The 1-step system has been further classified into the 2-bottle 1-step and 1-bottle 1-step systems, referred to as “all-in-one” systems (De Munck et al 2005; Van Meerbeek et al 2005). These adhesives have then been further classified according to their acidity; strong (pH <1), immediately strong (pH = 1.0-2.0), and mild (pH >2) (Fig. 1-2).. 7.
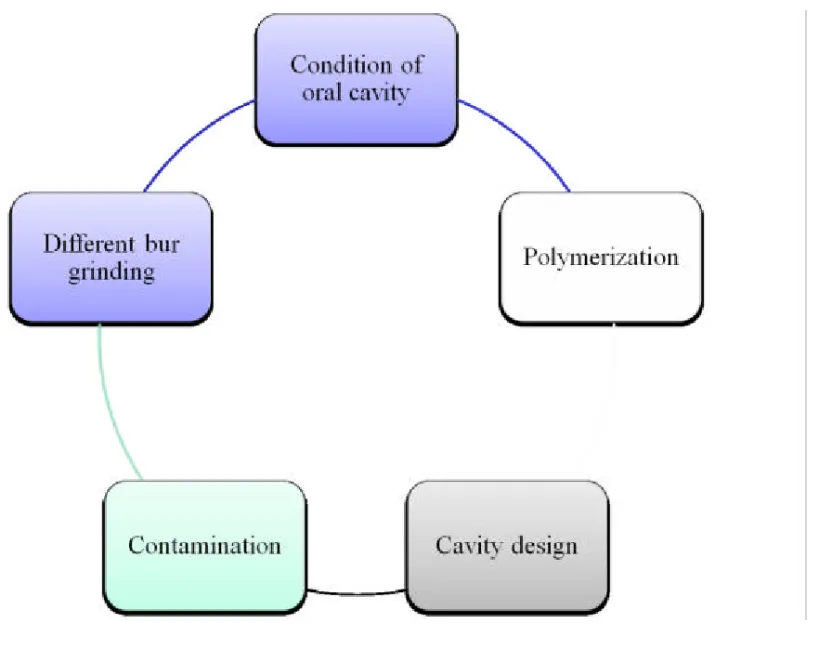
(9) 1.3.. Clinical factors influencing resin-dentin bonding. To treat periodontal disease, we can evaluate the treated effects objectively by comparing pocket depth, bleeding rate on probing, tooth movement, microbiological testing, and visual characteristics by, for example, X-ray and photographs. In the case of removable denture prosthodontics, patient feeling may be the most important aspect of the clinical evaluation. In the case of adhesive restoration, however, in which adherence is the most important factor, bond strength between the prepared cavity and restorative material cannot be measured directly and objectively, e.g., the conditions of oral cavity, the polymerizations, the cavity designs, the contaminations and the different bur grindings. Therefore, treatment sets out simply to produce as good adherence and restoration as possible in each case (Fig. 1-3). 1.3.1. Condition of the oral cavity Certainly, it is important which adhesive material is selected. However, it is more important how the material is used. In principle, we must use it according to the manufacturer’s instruction after the caries infected tissue is removed entirely. However, we must also consider aspects of the oral cavity environment that are known to influence its bonding performance: Warmth and moisture of the oral cavity are reported to affect bond strength. Most laboratory studies have been performed at room temperature (25±2℃) and 50% relative humidity (RH). However, the environment in the oral cavity is approximately 30℃ and over 75%RH. The higher humidity has been reported by some to negatively affect bond strength (Burrow et al 1995; Miyazaki et al 2001). The rubber dam isolation technique is required to achieve good results, and importantly it also prevents contamination of the tooth cavity with saliva and blood. 1.3.2. Polymerization of adhesive resin/restored composites Sufficient polymerization also plays an important role in the outcome of restorations. Increasing the degree of conversion has been one of the most. 8.
(10) effective factors for improving contemporary adhesive resin systems, alongside increasing filler loading and developing adhesive monomers. Additionally, new light sources have recently been introduced to replace the traditional quartz-tungsten-halogen (QTH) light curing unit. The new light sources include the plasma-arc, light-emitting diode (LED), argon laser and xenon lamps. In particular, blue LED light curing units present advantages in that they are portable, cordless, and have a longer lifetime than QTH units (Fujibayashi et al 1996). Since the range and peak of the emitted wavelengths are different for each light source, the mechanical properties of the adhesive resin are influenced. 1.3.3. Cavity design The concept of the configuration factor (C-factor), which is the degree of disruption of the adhesive interface by cavity design due to contraction stress during polymerization, was initially proposed by Feilzer et al in 1987. Contraction stress is influenced by the ratio of bonded to unbonded free surface area. As the C-factor increases, step/pulsed curing or use of a stress absorbing liner with flowable composite become effective ways to reduce marginal gaps from polymerization shrinkage (Albers 2002) 1.3.4. Contamination Contamination of a cavity by saliva, blood and gingival fluid is one of the clinical factors affecting resin bonding (Hiranuma et al 1992; Hebling and Feigal 2000; Hiraishi et al 2003; Sattabanasuk et al 2006; Shiraishi 1998). These contaminants decrease bond strengths and resin-tooth interfacial adaptation. When not carrying out bonding, isolation with a rubber dam in place is highly recommended to avoid contaminating the cavity. 1.3.5. Different bur grinding Selection of a bur is also important to consider in relation to dentin bond strength. Several reports suggest the influence of smear layer thickness on bond strength, and this factor will be presented in detail in 1.4.. 9.
(11) Restoration that accounts for the above-mentioned clinical factors which affect adherence to the restorative materials should prove satisfactory. 1.4.. Influence of smear layer on dentin bonding. The smear layer has been defined as a layer of debris on the surface of dental tissues created by cutting a tooth (Eick et al. 1970) and contains cut collagen fibers and hydroxyapatite crystallites (Guinnett 1984). It adheres weakly to the underlying dental tissues but cannot be removed by ordinary water spray. Not only are smear layers usually contaminated with microorganisms, but also any remainder of the layer causes a weakness of resin bonding because it interferes with monomer penetration (Tao et al 1988). Thus it should be dissolved and removed using acidic conditioner before resin bonding (Tao et al 1988; Fusayama et al 1979; Toida et al 1995; Tagami et al 1981; Kanemura et al, 1999; Watanabe et al 1994b; Nakabayashi and Saimi 1994; Koibuchi et al 2001). On the other hand, especially in dentin, excess acid conditioning also causes a weakness of bonding (Hashimoto et al 2002, Kameyama et al 2004). Excess demineralization of the superficial dentin dissolves and removes the inorganic matrix, exposing the collagen network. Exposed demineralized collagen will collapse due to denaturing by the acid conditioning and subsequent air dry (Igarashi 1997), and this might result in insufficient infiltration of the resin monomer into the demineralized area. The nature of the smear layer depends on the roughness of abrasive paper or bur used, speed of abrasion, and pressure applied (Semeraro et al 2006). Generally, coarse abrasive materials create a thicker smear layer. The difference of abrasive roughness affects bond strength, but its effect depends on the acidity of the adhesive system itself (Ogata et al 2001, 2002; Semeraro et al 2004; Koase et al 2004a, 2004b; Pansrisomboon et al 2007; Tay et al 2000a, 2000b). Ogata and colleagues investigated the effect of different smear layers on tensile bond strengths between dentin and three mild self-etch adhesives (Ogata et al 2001) and found that micro-tensile bond strength of regular-grit diamond bur-cut dentin was significantly lower than #600 silicon-carbide paper-ground dentin for all of the self-etch adhesives tested. On the other hand, in another of their reports, no significant difference was found between diamond. 10.
(12) bur-cut dentin and #600 silicon-carbide paper-ground dentin in Single Bond etch & rinse adhesive (Ogata et al 2001). Similar results are also reported for bond strength of adhesive resin cements in indirect enamel/dentin bonding (Koase et al 2004b).. 1.5.. Resin-coating method for indirect restorations. Several studies have recently reported the effectiveness of the resin-coating technique for indirect restorations. This technique was first proposed by Masaka (1990) using the 4-META/MMA-TBB resin system (Superbond C&B, Sun Medical) and was developed by Yasuda (1992). Farthermore, Satoh et al (1994) subsequently presented details of this technique for clinical use. using a two-step self-etching system (Clearfil Liner Bond II, Kuraray Medical). Resin coating minimizes pulpal irritation and postoperative sensitivity, increases initial and durable bond strength, and prevents micro leakage (Tagami et al 1999; Nikaido et al 2003a, 2003b; Kitasako et al 2002; Jayasooriya et al 2003a, 2003b; Maruoka et al 2007; Udo et al 2007; Okuda et al 2007; Kosaka et al 2005; Momoi et al 2003). Although the influences of temporary filling materials or impression materials on bond strengths have been evaluated while taking into account the clinical situation, the influence of different bur grinding on bond strength to resin-coated and indirect bonded dentin has not been reported. Therefore, in the next chapter, the influence of different bur grinding on micro-tensile bond strengths to resin-coated and indirect bonded dentin is investigated using two different types of two-step adhesives.. 1.6.. References. Albers HF. Tooth-colored restoratives: Principles and techniques. 9th Edition, BC Decker, Hamilton, London, UK, 2002. Black GV. Principals of cavity preparation. In: G.V. Black’s work on Operative Dentistry Vol. 2 Technical procedures in making restorations in the teeth (7th Edition). Henry Kimpton, London, 1936.. 11.
(13) Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surface. J Dent Res 1955: 34; 849-853. Burrow MF, Taniguchi Y, Nikaido T, Satoh T, Inai N, Tagami J, Takatsu T. Influence of temperature and relative humidity on early bond strengths to dentin. J Dent 1995; 23: 41-45. De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, Van Meerbeek B. A critical review of the durability of adhesion to tooth tissue: Methods and results. J Dent Res 2005; 84: 118-132. Eick JD, Wilko RA, Anderson CH, Sorensen SE. Scanning electron microscopy of cut tooth surfaces and identification of debris by use of the electron microscope. J Dent Res 1970; 49(6): 1359-1368. Feilzer A, De Gee AJ, Davidson CL. Setting stress in composite resin in relation to configuration of the restoration. J Dent Res 1987; 66: 1636-1639. Fusayama T. Outline of Operative Dentistry, 1st Edition, Nagasue Shoten, Tokyo, 1996. Fusayama T, Nakamura M, Kurosaki N, Iwaku M. Nonpressure adhesion of a new adhesive restorative system. J Dent Res 1979; 58: 1364-1370. Fusayama T, Nakamura M, Kurosaki N, Iwaku M. Non-pressure adhesion of a new adhesive restorative system. J Dent Res 1980; 58: 1364-1370. Fujibayashi K, Ishimaru K, Kohno A. Newly developed light-activation unit using blue light-emitting diodes. Part 1 A fundamental study. Jpn J Conserv Dent 1996; 39: 180-188. Gwinnett AJ. Smear layer: Morphological considerations. Oper Dent 1984; Suppl 3, 2-12. Hashimoto M, Ohno H, Kaga M, Sano H, Tay FR, Oguchi H, Araki Y, Kubota M.. 12.
(14) Over-etching effects on micro-tensile bond strength and failure patterns for dentin bonding system. J Dent 2002; 30: 99-105. Hebling J, Feigal RJ. Use of one-bottle adhesive as an intermediate bonding layer to reduce sealant microleakage on saliva-contaminated enamel. Am J Dent 2000; 13: 187-191. Hiraishi N, Kitasako Y, Nikaido T, Nomura S, Burrow MF, Tagami J. Effect of artificial saliva contamination on pH value change and dentin bond strength. Dent Mater 2000; 19: 429-434. Hiranuma K, Watanabe I, Nakabayashi N. Effect of saliva contamination on adhesion of 4-META/MMA-TBB resin to teeth pretreated with 10-3. Adhes Dent 1992; 10: 197-202. Igarashi K, Toida T, Nakabayashi N. Effect of Phenyl-P/HEMA primer on bonding to demineralized dentin by phosphoric acid. J Jpn Dent Mater 1997; 16: 55-60. Islam MR, Takada T, Weerasinghe DS, Uzzaman MA, Foxton RM, Nikaido T, Tagami J. Effect of resin coating on adhesion of composite crown restoration. Dent Mater J 2006; 25: 272-279. Jayasooriya PR, Pereira PNR, Nikaido T, Tagami J. Efficacy of a resin coating on bond strengths to resin cement to dentin. J Esthet Restor Dent 2003; 15: 105-113. Jayasooriya PR, Pereira PNR, Nikaido T, Burrow MF, Tagami J. The effect of a “resin coating” on the interfacial adaptation of composite inlays. Oper Dent 2003; 28: 28-35. Kameyama A, Muto Y, Nakazawa Y, Kawada E, Oda Y, Hirai Y. Resin bond strengths to over-etched dentin: influences of fluoride releasing from adhesive resin and storage into the mineralized solution. Jpn J Conserv Dent 2004; 47: 403-410. Kanemura N, Sano H, Tagami J. Tensile bond strength and SEM evaluation of. 13.
(15) ground and intact enamel surface. J Dent 1999; 27: 523-530. Kanca J. Effect of resin primer solvents and surface wetness on resin composite bond strength to dentin. Am J Dent 1992; 5: 213-215. Kitasako Y, Burrow MF, Nikaido T, Tagami J. Effect of resin-coating technique on dentin tensile bond strengths over 3 years. J Esthet Restor Dent 2002; 14: 115-122. Koase K, Inoue S, Noda M, Tanaka T, Kawamoto C, Takahashi A, Nakaoki Y, Sano H. Effect of bur-cut dentin on bond strength using two all-in-one and one two-step adhesive systems. J Adhes Dent 2004; 6: 97-104. Koase K, Inoue S, Komatsu H, Sano H. Bond strength of resin cements and adhesive systems to bur-prepared tooth substrates. Jpn J Conserv Dent 2004; 47(1); 87-109. Koibuchi H, Yasuda N, Nakabayashi N. Bonding to dentin with a self-etching primer: the effect of smear layers. Dent Mater 2001; 17: 122-126. Kosaka S, Kajihara H, Kurashige H, Tanaka T. Effect of resin coating as a means of preventing marginal leakage beneath full cast crowns. Dent Mater J 2005; 24: 117-122. Maruoka R, Nikaido T, Ikeda M, Foxton RM, Tagami J. Effect of resin-coating technique on coronal leakage inhibition in endodontically treated teeth. Int Chin J Dent 2007; 7(1); 1-6. Masaka N. A study of protective coating of exposed dentine. Adhes Dent 1990; 8: 137. Misu M. A clinico-pathological study of pulp response to a composite resin restoration system using adhesive bonding agent. Shikwa Gakuho 1981; 81: 47-82. Miyasaka K, Nakabayashi N. Combination of EDTA conditioner and. 14.
(16) phenyl-P/HEMA self-etching primer for bonding to dentin. Dent Mater 1999; 15: 153-157. Miyazaki M, Rikuta A, Tsubota K, Yunoki I, Onose H. Influence of environmental conditions on dentin bond strengths of recently developed dentin bonding systems. J Oral Sci 2001; 43:35-40. Momoi Y, Akimoto N, Kida K, Yip KH-K, Kohno A. Sealing ability of dentin coating using adhesive resin systems. Am J Dent 2003; 16: 105-111. Munksgaard EC, Asmussen E. Bond strength between dentin and restorative resins mediated by mixture of HEMA and glutaraldehyde. J Dent Res 1984; 63: 1087-1089. Nakabayashi N. Resin reinforced dentin due to infiltration of monomers into the dentin at the adhesive interface. J Jpn Dent Mater 1982; 1: 78-81. Nakabayashi N, Saimi Y. Bonding to intact dentin. J Dent Res 1996; 75: 1706-1715. Nikaido T, Cho E, Nakajima M, Tashiro H, Toba S, Burrow MF, Tagami J. Tensile bond strengths of resin cements to bovine dentin using resin coating. Am J Dent 2003a; 16: 41A-46A. Nikaido T, Nakaoki Y, Ogata M, Foxton R, Tagami J. The resin-coating technique. Effect of a single-step bonding system on dentin bond systems. J Adhes Dent 2003b; 5: 293-300. Nikaido T, Yoda A, Foxton RM, Tagami J. A resin coating technique to achieve minimal intervention in indirect resin composites: A clinical report. Int Chin J Dent 2003c; 3: 62-68. Ogata M, Okuda M, Yamaguchi S, Nakajima M, Pereira PNR, Tagami J. Effects of different burs on dentin bond strengths of self-etching primer bonding systems. Oper Dent 2001; 26: 375-382.. 15.
(17) Ogata M, Harada N, Yamaguchi S, Nakajima M, Tagami J. Effect of self-etching primer vs. phosphoric acid etchant on bonding to bur prepared dentin. Oper Dent 2002; 27: 447-454. Okuda M, Nikaido T, Maruoka R, Foxton RM, Tagami J. Microtensile bond strengths to cavity floor dentin in indirect composite restorations using resin coating. J Restor Esthet Dent 2007; 19: 38-48. Pangsrisomboon B, Harnirattisai C, Nilsri K, Burrow MF. Microtensile bond strength of self-etching adhesive systems to differently prepared dentin. Am J Dent 2007; 20: 259-262. Satoh M, Inai N, Nikaido T, Tagami J, Inokoshi S, Yamada T, Takatsu T. How to use Liner Bond System as a dentin and pulp protector in indirect restorations. Adhes Dent 1994; 12: 41-47. Sattabanasuk V, Shimada Y, Tagami J. Effects of saliva contamination on dentin bond strength using all-in-one adhesives. J Adhes Dent 2006; 8: 311-318. Semeraro S, Mezzanzanica D, Spreafico D, Gagliani M, Re D, Tanaka T, Sidhu SK, Sano H. Effect of different bur grinding on the bond strength of self-etching adhesives. Oper Dent 2006; 31(3): 317-323. Shiraishi M. Analysis of blood-contaminated dentin surface and the influence of blood contamination on adhesive restorations. Jpn J Conserv Dent 1998; 41: 236-252. Tagami J, Tao L, Pashley DH, Hosoda H, Shono H. Effects of high speed cutting on dentin permeability and bonding. Dent Mater 1991; 7: 234-239. Tagami J, Kitasako Y, Sonoda H. Pulp protection and restoration with adhesive resin. Adhes Dent 1999; 17: 56-60. Tao L, Pashley DH, Boyd L. The effect of different types of smear layers on dentin and enamel bond strength. Dent Mater 1988; 4: 208-216.. 16.
(18) Tay FR, Gwinett AJ, Wei SHY. Micromorphological spectrum from overdrying to overwetting acid-conditioned dentin in water-free, acetone-based, single bottle primer/adhesives. Dent Mater 1996; 12: 236-244. Tay FR, Sano H, Carvalho R, Pashley EL, Pashley DH. An ultrastructural study of the influence of acidity of self-etching primers and smear layer thickness on bonding to intact dentin. J Adhes Dent 2000a; 2: 83-98. Tay FR, Carvalho R, Sano H, Pashley DH. Effect of smear layers on the bonding of a self-etching primer to dentin. J Adhes Dent 2000b; 2: 99-116. Toida T, Watanabe A, Nakabayashi N. Effect of smear layer on bonding to dentin prepared with bur. J Jpn Dent Mater 1995; 14: 109-116. Udo T, Nikaido T, Ikeda M, Weerasinghe DS, Harada N, Foxton RM, Tagami J. Enhancement of adhesion between resin coating materials and resin cements. Dent Mater J 2007; 26: 519-525. Van Meerbeek B, Van Landuyt K, De Munck J, Hashimoto M, Peumans M, Lambrechts P, Yoshida Y, Inoue S, Suzuki K. Technique-Sensitivity of Contemporary Adhesives. Dent Mater J 2005; 24: 1-13. Watanabe I, Nikaido T, Nakabayashi N. Effect of adhesion promoting monomers on adhesion to ground dentin. J Jpn Dent Mater 1990; 9: 888-893. Watanabe I, Nakabayashi N, Pashley DH. Bonding to ground dentin by a phenyl-P self-etching primer. J Dent Res 1994a; 73: 1212-1220. Watanabe I, Saimi Y, Nakabayashi N. Effect of smear layer on bonding to ground dentin: Relationship between grinding condition and tensile bond strength. J Jpn Dent Mater 1994b; 13: 101-108. Yasuda N. Temporary sealing. Adhes Dent 1992; 10: 245-246.. 17.
(19) Chapter 2. Influence of different bur grinding on micro-tensile bond strength in resin-coated dentin. 18.
(20) 2.0.. Abstract. Objectives: To determine the effect of different bur grinding on micro-tensile bond strength (µTBS) of two different types of adhesives to resin-coated dentin. Methods: Dentin surfaces were prepared from mid-coronal sound dentin in extracted human molars with two different diamond burs (regular-grit or superfine-grit). The surfaces were resin coated using UniFil Bond (UB) or Adper Single Bond (SB), followed by application of UniFil Flow, the flowable resin composite. Bonded to the surfaces were a polymerized disc of indirect resin composite (Gradia) with adhesive resin cement (Link Max) and also a polymethyl-methacrylate (PMMA) rod with 4-META/MMA-TBB resin (Superbond C&B). Specimens without resin coating (NC) were also produced as a control for each type of bur-grinded dentin. After storage for 24 hours in 37ºC distilled water, the bonded teeth were sectioned into slices (0.7-mm thick) perpendicular to the bonded surfaces. The specimens were then subjected to µTBS testing at a crosshead speed of 1.0 mm/min. Data were analyzed with one-way and two-way ANOVA, with statistical significance set at p=0.05. Results: When UB was bonded to dentin prepared using a regular-grit diamond bur, µTBS was significantly lower than that prepared using a super fine-grit bur. By contrast, when SB was bonded to dentin prepared using the regular-grit bur, µTBS was significantly higher than when using the super fine-grit bur. In NC specimens, no significant differences were found between the µTBS of two differently ground surfaces. Conclusion: Selection of bur type is important to improve the bond strength of adhesive resin cement between indirect resin composite material and resin-coated dentin. 2.1.. Introduction. In the early 1990’s the use of a resin-coating technique for indirect restorations was proposed in order to produce a hybrid layer and a tight sealing film on the prepared surface with an adhesive system and a low viscosity resin composite (Nikaido et al 1992; Otsuki et al 1993). This technique has recently been shown to be capable of not only increasing the bond strength of resin cement and producing good interfacial adaptation (Nikaido et al 2003a, 2003b; Kitasako et al 2002; Jayasooriya et al 2003), but also protecting the prepared dentin and. 19.
(21) underlying vital pulp tissue (Satoh et al 1994; Momoi et al 2003), thereby achieving minimally invasive restoration for clinical application (Nikaido et al 2003c). The success of recent direct and indirect restorative treatments trends to depend on their adhesive performance. However, several factors are also considered to affect their performance clinically, e.g., regional differences in dentin (dentin depth and/or detection of dentin tubule) (Burrow et al 1994; Shono et al 1999; Phrukkanon et al 1999; Inoue et al, 2001, 2003; Ogata et al 2001; Liu et al 2002; Yoshikawa et al 1999), cavity configuration (Feilzer et al 1987), temperature and relative humidity (Burrow et al 1995; Miyazaki et al 2001), dentin wettability (Finger et al 1994), saliva/blood contamination (Pashley et al 1988; Fritz et al 1998), storage condition of the adhesive system (Fujita and Nishiyama 2006; Nishiyama et al 2006), and degree of conversion and strength of adhesion itself (Takahashi et al 2002; Ikeda et al 2005). Different bur grinding has also been reported by some to affect bond strength (Ogata et al 2001, 2002; Semeraro et al 2006; Koase et al 2004a). The difference in bond strength created by different bur grinding is not due to the roughness of the dentin itself but to the smear layer thickness (Tao et al 1988, 2000a, 2000b; Koibuchi et al 2001; Yoshida et al 2004). These differences have been reported in both direct and indirect bonding (Koase et al 2004b). In indirect restoration, further factors might affect the bond strength because of the increased number of steps involved. These include differences of the coated adhesive system, application of low viscosity resin composite immediately after photocuring the adhesive resin, influences of the impression material, temporary filling material, and differences of luting resin cement. Different bur grinding may also affect the bond strength as it does in direct and indirect dentin bonding. The purpose of this study was, therefore, to evaluate the effect of different bur grinding on micro-tensile bond strength (µTBS) of one 2-step etch & rinse adhesive and one 2-step self-etch adhesive to resin-coated dentin. 2.2.. Materials and Methods. 2.2.1. Test Teeth. 20.
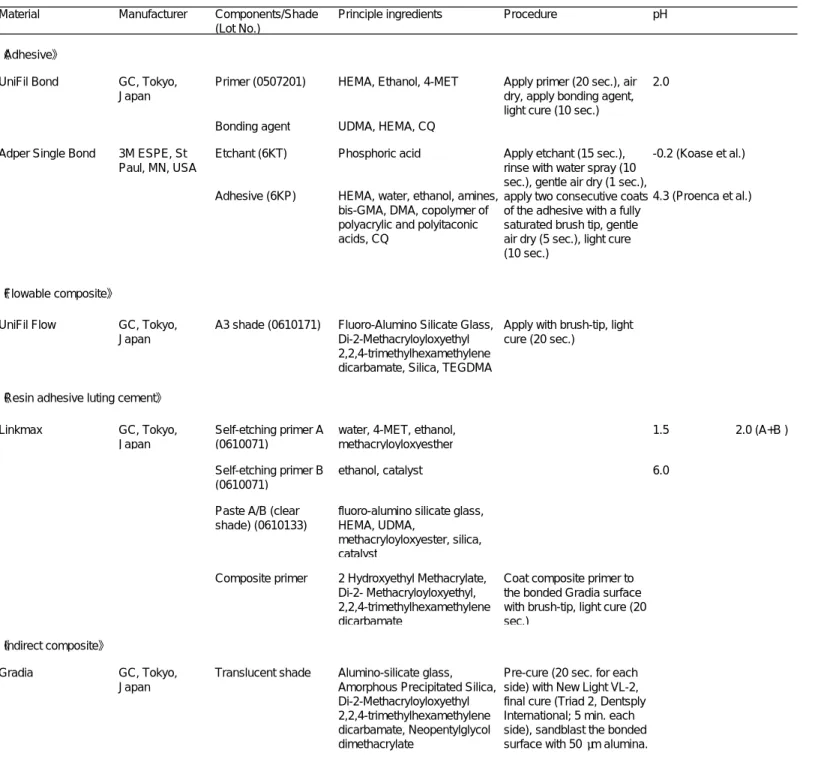
(22) Caries-free human molars, collected with patient informed consent under a protocol reviewed and approved by the Commission for Medical Ethics of Tokyo Dental College Chiba Hospital (No. 153), were stored in an aqueous solution of 0.5% Chloramine-T at 4 ºC, and used within three months of extraction. The coronal surfaces of the teeth were trimmed using a model trimmer (MT-7, J. Morita Co., Kyoto, Japan) to form a long, flat dentin surface at the mid-coronal portion. Each surface was ground with 600-grit silicon carbide paper under running water, and then ground with a regular-grit diamond bur (Diamond Point FG, #114, Shofu, Kyoto, Japan) connected to a 1:5 high-speed motor handpiece (Intramatic LUX-3, Kavo, Germany). Half of the specimens were further prepared with a superfine-grit diamond bur (Diamond Point FG, #SF 114, Shofu). The two types of dentin substrates were randomly assigned to each of the three groups (two coated adhesives and non-coated control). 2.2.2. Materials used and bonding procedures For the resin coating of indirect restorations, one two-step etch & rinse adhesive (Adper Single Bond, 3M ESPE, Minneapolis, MN, USA) and one two-step self-etch adhesive (UniFil Bond, GC, Tokyo, Japan) were used with a flowable resin composite, UniFil Flo (Shade A3, GC), in this experiment. The resin cement used in this study was Linkmax (Clear shade, GC). To prepare the indirect composite discs, Gradia (GC, Incisal shade) was filled in an acrylic ring of 9 mm diameter and 5 mm height, and pressed with two slide glasses, pre-cured with New Light VL-2 for 20 seconds each side, and then cured in Triad II (Dentsply International, York, PA, USA) for 10 minutes (5 minutes each side). After the polymerization, the Gradia slabs were sand-blasted with 50-µm alumina and rinsed with tap water. The sand-blasted surfaces were surface treated with Composite Primer (GC) and visible light-irradiated with New-light VL-2 (GC) for 20 seconds immediately prior to bonding. Each adhesive system was applied to the ground dentin surfaces according to the manufacturer’s instructions (see Table 2-1), and immediately thereafter,. 21.
(23) UniFil Flo was applied with a disposable micro-brush tip and light-cured (New Light VL-2) for 20 seconds. After wiping off the uncured layer with alcohol-contained cotton, the dentin surface was conditioned with the mixture of Linkmax self-etching primer A and B for 30 seconds, and gently air dried. Immediately after, the dentin surface was bonded to the Gradia slab with Linkmax. Ninety seconds later, the bonded interface was light cured with New-light VL-2 for 20 seconds, and further built up with a PMMA rod (8 x 8 x 3 mm) using 4-META/MMA-TBB resin (Superbond C&B, San Medical, Moriyama, Japan). Each light curing with New-light VL-2 was controlled to approximately 700 mW/cm2. Thirty minutes after the cementing, all specimens were stored in water at 37ºC for 24 hours. Thereafter, each bonded specimen was sectioned perpendicular to the bonded interface to obtain 4 or 5 slabs of 0.7 mm thickness. Each slab was then trimmed with a superfine diamond bur (#SF 114, Shofu) to obtain an hourglass shape so that narrowest portion at the interface was approximately 1.4 mm. The thickness of the bonded area of each specimen was then verified by a digital micrometer (Mitutoyo, Tokyo, Japan). Each specimen was attached to a Bencor Multi-T testing device (Danville Engineering Co, San Ramen, CA, USA) with cyanoacrylate adhesive (Model Repair II Blue, Dentsply-Sankin, Ohtawara, Japan) connected to a universal testing machine (Tensilon RTC-1150-TSD, Orientec, Tokyo, Japan) for micro-tensile bond strength (MTBS) testing at a crosshead speed of 1 mm/min. µTBS was derived by dividing the imposed force (N) at the time of fracture by the bond area (mm2). When a specimen failed during processing, µTBS was set at 0 MPa (De Munck et al, 2004). Data were analyzed by one-way and two-way analyses of variance (ANOVA) at a 5% level of significance. 2.2.3. Failure mode analysis For determining the modes of failure, both the dentin and composite halves of the fractured specimens were observed under a stereomicroscope (MS-803, Moritex, Tokyo, Japan) at 210x magnification. The mode of failure was classified into five categories: adhesive interfacial (fracture between the dentin or hybrid layer and the overlying adhesive), mixed R/A (mainly cohesive failure in. 22.
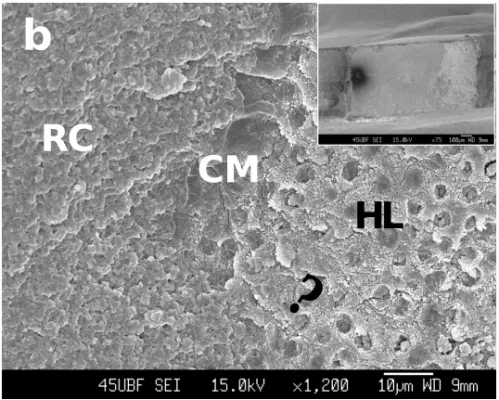
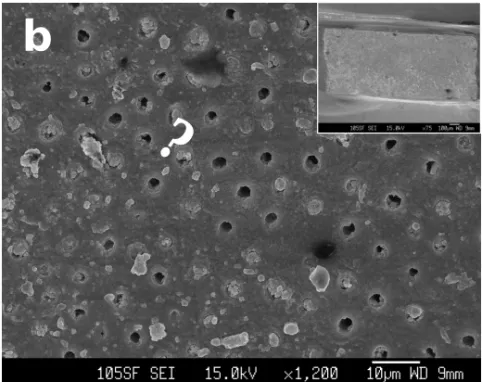
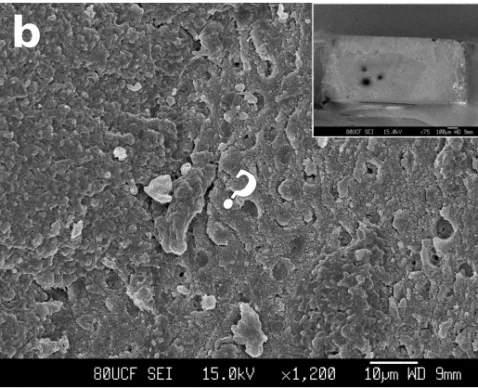
(24) dentin or resin material and partially adhesive interfacial failure in the same sample), mixed A/R (mainly interfacial and partially cohesive failure in dentin or resin material in the same sample), cohesive in resin (failure within adhesive, resin cement and/or Gradia), and cohesive in dentin. The most frequently observed failure mode and a µTBS close to the mean were observed by field-emission scanning electron microscopy (FE-SEM; JSM-6340F, JEOL, Tokyo, Japan). 2.3.. Results. Mean µTBS, standard deviations (SD), number of specimens (n), and number of pre-testing failures (PTF) of all evaluated groups are summarized in Table 2-2, and graphically presented in Fig. 2-2. While two-way ANOVA revealed that ‘adhesive system’ had a significant effect on MTBS (p < 0.0001), no significant difference was found for ‘surface grinding’ (p = 0.5442). However, both factors revealed a significant interaction on MTBS (p = 0.0011). Therefore, further analysis for significant differences between the groups was carried out using the Tukey-Kramer post-hoc test. To compare the bur types, in UniFil Bond, the µTBS of the superfine-grit bur was significantly higher than that of the regular-grit bur (p < 0.05). On the other hand, no significant difference was found between the two bur types in Single Bond (p > 0.05). However, more than half of the superfine-grit specimens (16/28) failed during processing. Also, no significant difference was found between regular-grit and superfine-grit in the non-coated control (p > 0.05). Distribution of failure modes is summarized in Fig. 2-3, and representative SEM photographs of the fractured surfaces after the µTBS testing in each group are shown in Figs. 2-4, 2-5, and 2-6. In UniFil Bond, the percentage of failure at the coated resin was higher for superfine-grit than for regular-grit. Almost all dentinal tubules found at the failed surface were plugged with coated adhesive. In Single Bond, almost all specimens failed at the adhesive interface or showed mixed failure mainly due to interfacial failure. Different from UniFil Bond, the fractured surface at the interfacial site in Single Bond showed opened dentinal tubules. More than half of the specimens showed interfacial failure for both regular-grit and superfine-grit bur preparation, but almost all dentinal tubules. 23.
(25) were plugged with resin cement. 2.4.. Discussion. Several factors have been reported to affect bond strength to resin-coated dentin, namely, the adhesive system itself, combined application of a low-viscosity flowable composite and adhesive system, resin cement, and tooth substrate. In this study, the influence of two factors, different bur grinding and the adhesive system, on µTBS between dentin and indirect resin composite was evaluated. In non-coated dentin, no significant difference was found between regular-grit prepared dentin and superfine-grit prepared dentin (p > 0.05). Linkmax categorized as a self-etch resin cement, and acidity of self-etching primer was mild (pH = 2.0). Koase et al (2004b) also determined the µTBS of Linkmax to both regular-grit prepared and superfine-grit prepared dentin, and, contrary to the present results, found that superfine-grit produced a significantly higher µTBS than regular-grit. In their study, however, 6 of 16 superfine-grit prepared dentin specimens failed before µTBS testing, although no regular-grit prepared specimens failed. Since they excluded the data of pre-test failure when calculating mean µTBS, the present results should not be interpreted as different from their results. Superfine-grit preparation produced significantly higher µTBS than regular-grit in UniFil Bond-coated dentin. The influence of dentin abrasive roughness on µTBS under direct bonding of resin composite has been reported by some groups (Ogata et al 2001, 2002; Semeraro et al 2006). Ogata et al (2001) reported that µTBS of regular-grit diamond bur-cut dentin to direct bonded resin composite was significantly lower than that of #600 silicon-carbide paper-ground dentin for each self-etch adhesive tested. Tay et al (2000b) reported that µTBS of direct bonded resin composite using Clearfil SE Bond (Kuraray Medical) 2-step self-etch adhesive to #60-grit silicon-carbide paper-ground dentin was significantly lower than that to #180- and #600-grit ground dentin. They also demonstrated the existence of a hybridized smear layer immediately above the hybrid layer due to penetration of adhesive monomer into the partially demineralized smear layer. Semeraro et al (2006) also reported higher µTBS of direct resin bonding to superfine-grit prepared dentin than to regular-grit prepared dentin when using Clearfil SE Bond, and based on their SEM findings. 24.
(26) they suggested that the greater porosity of intertubular dentin with the superfine-grit preparation implied more channels of penetration of adhesive monomers. The results obtained in the present study might be due to the same reason, because the acidity of the self-etching primer contained in UB was the same as that in Clearfil SE Bond (pH=2.0). On the other hand, Koase et al. (2004b) found no significant difference of µTBS between regular-grit and superfine-grit prepared dentin when using Clearfil Protect Bond (known as Clearfil Megabond FA in Japan), although the pH of its self-etching primer was same as Clearfil SE Bond. They attribute the results to differences in monomer diffusion and mechanical strength of the adhesive itself. In our previous study, tensile bond strength of a specimen primed with SE Bond primer and bonded with Protect Bond (Kuraray Medical) adhesive was significantly lower than the specimen primed with SE Bond primer and bonded with SE Bond adhesive (Kameyama et al 2001), and this data supports their speculation. In Single Bond, however, no significant difference was found between regular-grit and superfine-grit prepared dentin. These results are similar to those of Ogata et al’s (2002) study of direct bonding. It is worthy of note that 16 of 28 superfine-grit prepared specimens failed before µTBS testing, suggesting the existence of a resin-unprotected demineralized layer beneath the hybrid layer. A previous study by Spencer et al (1999) found a 4 µm-thick layer of unprotected protein immediately under the 2 µm-thick hybrid layer when the dentin was prepared by #600 silicon carbide paper and bonded with Single Bond. Once the resin monomer has sufficiently penetrated into the demineralized and exposed protein layer, a higher µTBS can be expected. Inversely, insufficient penetration might cause of a degradation of its adhesion and serious gap formation. Although resin-coating with UniFil Bond for superfine-grit prepared dentin significantly contributed to the increase in µTBS, that with Single Bond showed no such effect. Nikaido et al (2003a) also reported a significant effect of resin coating in the UniFil Bond/Link Max combination, which was not found in the Single Bond/Rely X (3M) combination. Resin coating with Single Bond should really be avoided, since opening of dentinal tubules at the fractured surface and. 25.
(27) a large number of pre-test failures might suggest a cause of bacterial invasion into the deep dentin and pulpal tissue. On the other hand, in regular-grit prepared dentin, there was no significant effect of resin coating in either UniFil Bond or Single Bond. These results suggest that selections of both the coated resin and the grinding bur are important for achieving good clinical results of indirect bonded restoration. This study evaluated the different types of two-step adhesives as resin-coating materials. Current adhesive research has focused on simplifying the application procedure, to etch, prime and bond as one-step. These one-step self-etch adhesives can be further classified by acidity as ‘mild’ (pH>2), ‘intermediately mild’ (pH=1-2) and ‘strong’ (pH<1) (Van Meerbeek et al 2005; Koshiro et al 2006). The bond strength of superfine-grit prepared dentin and direct bonded composite with ‘strong’ 1-step adhesive reportedly produces a large number of failures during specimen fabrication (Semeraro et al 2006), as occurred with Single Bond in the present study. In contrast, ‘mild’ 1-step adhesive is suggested to leave a residual smear layer at the adhesive interface. Because these mild adhesives contain larger amount of solvents such as water, ethanol and acetone, weaker mechanical strengths of the polymerized adhesive itself compared to 2-step self-etch adhesives have been reported by some groups (Ikeda et al 2005b; Reis et al 2005). Therefore, the hybridized area between the adhesive and residual smear layer may bring about defects of the adhesive interface. Further studies are needed to clarify the influence of different bur grinding on bond strength to resin-coated dentin. 2.5.. Conclusions. Within the limitations of this study, the following conclusions are drawn. 1. Superfine-grit preparation of dentin surface was affected by resin-coating with a 2-step self-etch adhesive. 2. Superfine-grit preparation of dentin surface somewhat decreased the micro-tensile bond strength when resin-coated with a 2-step etch-and-rinse adhesive. 3. Selection of bur did not affect the micro-tensile bond strength when the resin-coating technique was not applied.. 26.
(28) 2.6.. References. Burrow MF, Takakura H, Nakajima M, Inai N, Tagami J, Takatsu T. The influence of age and depth of dentin on bonding. Dent Mater 1994; 10: 241-246. Burrow MF, Taniguchi Y, Nikaido T, Satoh T, Inai N, Tagami J, Takatsu T. Influence of temperature and relative humidity on early bond strengths to dentin. J Dent 1995; 23: 41-45. Feilzer A, De Gee AJ, Davidson CL. Setting stress in composite resin in relation to configuration of the restoration. J Dent Res 1987; 66: 1636-1639. Finger WJ, Inoue M, Asmussen E. Effect of wettability of adhesive resins on bonding to dentin. Am J Dent 1994; 7: 35-38. Fritz UB, Finger WJ, Stern H. Salivary contamination during bonding procedures with a one-bottle adhesive system. Quintessence Int 1998; 29: 567-572. Fujita K, Nishiyama N. Degradation of single bottle type self-etching primer effectuated by the primer's storage period. Am J Dent 2006; 19: 111-114. Hiraishi N, Kitasako Y, Nikaido T, Nomura S, Burrow MF, Tagami J. Effect of artificial saliva contamination on pH value change and dentin bond strength. Dent Mater 2000; 19: 429-434. Ikeda T, De Munck J, Shirai K, Hikita K, Inoue S, Sano H, Lambrechts P, Van Meerbeek B. Effect of fracture strength of primer-adhesive mixture on bonding effectiveness. Dent Mater 2005; 21: 413-420. Kameyama A, Shuto S, Muto Y, Sazuka H, Ushiki T, Hosaka M, Hirai Y. Studies on an MDPB containing experimental resin bonding system. J Jpn Conserv Dent 2001; 44: 311-317. Koase K, Inoue S, Noda M, Tanaka T, Kawamoto C, Takahashi A, Nakaoki Y, Sano H. Effect of bur-cut dentin on bond strength using two all-in-one and one two-step adhesive systems. J Adhes Dent 2004a; 6: 97-104.. 27.
(29) Koase K, Inoue S, Komatsu H, Sano H. Bond strength of resin cements and adhesive systems to bur-prepared tooth substrates. Jpn J Conserv Dent 2004b; 47; 87-109. Koibuchi H, Yasuda N, Nakabayashi N. Bonding to dentin with a self-etching primer: the effect of smear layers. Dent Mater 2001; 17: 122-126. Koshiro K, Sidhu SK, Inoue S, Ikeda T, Sano H. New concept of resin-dentin interfacial adhesion: the nanointeraction zone. J Biomed Mater Res B Appl Biomater 2006; 77: 401-418. Liu J, Hattori M, Hasegawa K, Yoshinari M, Kawada E, Oda Y. Effect of tubule orientation and dentin location on the microtensile strength of bovine root dentin. Dent Mater J 2002; 21: 73-82. Miyazaki M, Rikuta A, Tsubota K, Yunoki I, Onose H. Influence of environmental conditions on dentin bond strengths of recently developed dentin bonding systems. J Oral Sci 2001; 43:35-40. Momoi Y, Akimoto N, Kida K, Yip KH-K, Kohno A. Sealing ability of dentin coating using adhesive resin systems. Am J Dent 2003; 16: 105-111. Nikaido T, Takada T, Burrow MF, Tagami J. Early bond strengths of dual cured resin cements to enamel and dentine. J Jpn Dent Mater 1992; 11: 910-915. Nikaido T, Cho E, Nakajima M, Tashiro H, Toba S, Burrow MF, Tagami J. Tensile bond strengths of resin cements to bovine dentin using resin coating. Am J Dent 2003a; 16: 41A-46A. Nikaido T, Nakaoki Y, Ogata M, Foxton R, Tagami J. The resin-coating technique. Effect of a single-step bonding system on dentin bond systems. J Adhes Dent 2003b; 5: 293-300. Nikaido T, Yoda A, Foxton RM, Tagami J. A resin coating technique to achieve minimal intervention in indirect resin composites: A clinical report. Int Chin J Dent. 28.
(30) 2003c; 3: 62-68. Nishiyama N, Tay FR, Fujita K, Pashley DH, Ikemura K, Hiraishi N, King NM. Hydrolysis of functional monomers in a single-bottle self-etching primer-correlation of 13C NMR and TEM findings. J Dent Res 2006; 85: 422-426. Ogata M, Okuda M, Nakajima, M, Pereira PNR, Sano H, Tagami J. Influence of the direction of tubules on bond strength to dentin. Oper Dent 2001a; 26: 27-35. Ogata M, Okuda M, Nakajima M, Pereira PNR, Tagami J. Effects of different burs on dentin bond strengths of self-etching primer bonding systems. Oper Dent 2001b; 26: 375-382. Ogata M, Harada N, Yamaguchi S, Nakajima M, Tagami J. Effect of self-etching primer vs. phosphoric acid etchant on bonding to bur prepared dentin. Oper Dent 2002; 27: 447-454. Otsuki M, Yamada T, Inokoshi S. Establishment of a composite resin inlay technique: Part 7. Use of low viscous resin. Jpn J Conserv Dent 1993; 36: 1324-1330. Pangsrisomboon B, Harnirattisai C, Nilsri K, Burrow MF. Microtensile bond strength of self-etching adhesive systems to differently prepared dentin. Am J Dent 2007; 20: 259-262. Phrukkanon S, Burrow MF, Tyas MJ. The effect of dentine location and tubule orientation on the bond strengths between resin and dentine. J Dent 1999; 27: 265-274. Reis A, Grandi V, Carlotto L, Bortoli G, Patzlaff R, Rodrigues Accorinte Mde L, Dourado Loguercio A. Effect of smear layer thickness and acidity of self-etching solutions on early and long-term bond strength to dentin. J Dent 2005; 33: 549-559. Satoh M, Inai N, Nikaido T, Tagami J, Inokoshi S, Yamada T, Takatsu T. How to. 29.
(31) use Liner Bond System as a dentin and pulp protector in indirect restorations. Adhes Dent 1994; 12: 41-47. Semeraro S, Mezzanzanica D, Spreafico D, Gagliani M, Re D, Tanaka T, Sidhu SK, Sano H. Effect of different bur grinding on the bond strength of self-etching adhesives. Oper Dent 2006; 31: 317-323. Shiraishi M. Analysis of blood-contaminated dentin surface and the influence of blood contamination on adhesive restorations. Jpn J Conserv Dent 1998; 41: 236-252. Shono Y, Ogawa T, Terashita M, Carvalho RM, Pashley EL, Pashley DH. Regional measurement of resin-dentin bonding as an array. J Dent Res 1999; 78: 699-705. Spencer P, Swafford JR, Unprotected protein at the dentin-adhesive interface. Quintessence Int 1999; 30: 501-507 Takahashi A, Sato Y, Uno S, Pereira PN, Sano H. Effects of mechanical properties of adhesive resins on bond strength to dentin. Dent Mater 2002; 18: 263-268. Tay FR, Sano H, Carvalho R, Pashley EL, Pashley DH. An ultrastructural study of the influence of acidity of self-etching primers and smear layer thickness on bonding to intact dentin. J Adhes Dent 2000a; 2: 83-98. Tay FR, Carvalho R, Sano H, Pashley DH. Effect of smear layers on the bonding of a self-etching primer to dentin. J Adhes Dent 2000b; 2: 99-116. Tao L, Pashley DH, Boyd L. The effect of different types of smear layers on dentin and enamel bond strength. Dent Mater 1988; 4: 208-216. Van Meerbeek B, Van Landuyt K, De Munck J, Hashimoto M, Peumans M, Lambrechts P, Yoshida Y, Inoue S, Suzuki K. Technique-Sensitivity of Contemporary Adhesives. Dent Mater J 2005; 24: 1-13.. 30.
(32) Yoshida E, Uno S. Voids formation along the bonding interface between a smeared dentin surface and all-in-one adhesives. Dent Mater J 2004; 23:643-649. Yoshikawa T, Sano H, Burrow MF, Tagami J, Pashley DH. Effects of dentin depth and cavity configuration on bond strength. J Dent Res 1999; 78: 898-905.. 31.
(33) Chapter 3. General discussion and conclusions. 32.
(34) Chapter 3 3.1.. General discussion and conclusions. Indirect vs. direct restorations: which is more reliable for posterior teeth?. The longevity of durability of a restorative material is an important factor in determining its efficacy as a treatment for dental caries and other defects of teeth. However, it remains a matter of conjecture. Dental amalgam has been the most extensively used posterior restorative material, due to its simple handling procedures, good physical properties, and documented clinical success over a century of use. In 1998, Collins et al reported the clinical performance of three types of direct composites, using amalgam restorations as controls. At the 8-year recall, 13.7% of the direct composite restorations had failed, as opposed to 5.8% of the amalgam restorations. However, any practical application of longevity data is somewhat offset by the fact that composite materials, including adhesive systems, are being modified or superseded almost constantly, thereby mitigating the benefits of long-term studies. Baratieri and Ritter (2001) reported the 4-year clinical performance of Class I and Class II direct composite restorations, finding that although 2.5% of the restorations had clinically detectable marginal fracture, none required replacement. More recently, Akimoto et al (2007) reported the 10-year long-term clinical evaluation of anterior and posterior restoration with the Clearfil Liner Bond 2 (Kuraray Medical) 2-step self-etch adhesive system. While their study showed slight marginal changes in clinical function in most cases, these changes were not clinically severe according to United States Public Health Service (USPHS) criteria and they concluded that placement of the Clearfil Liner Bond 2 was demonstrated to be acceptable for the clinical restoration of human teeth following 10 years of clinical function. Indirect resin-based composite restorations are often assumed to have superior clinical performance because of the improvements in laboratory-tested mechanical properties, such as decreased shrinkage and fracture toughness. However, the 11-year follow-up results of van Dijken (2000) concluded that the differences in longevity were not statistically significant. A major defect of indirect restoration is its low bond strength to dentin. Jayasooriya et al (2003) reported that µTBS between indirect resin composite and dentin bonded with. 33.
(35) Panavia F (Kuraray Medical) adhesive resin cement was significantly lower than that of direct resin composite bonded with Clearfil SE Bond (Kuraray Madical), and lower bond strength in indirect restoration could not improve to a similar level to that in direct composite restoration even if the resin-coating technique were applied. Therefore, direct composite restorations should be the first treatment of choice for posterior restorations. However, in certain situations, for example when large restorations are required, indirect restorations using a resin coating technique should be selected. Furthermore, the selection of materials (restorative materials, resin-coating materials and resin cements), bur, temporary material and impression material are all important factors in adhesive performance. 3.2.. General conclusion. This study found that the selections of a cavity-prepared bur and resin-coating material affected the micro-tensile bond strength between dentin and indirect composite material. Therefore, clinicians should be cognizant of the fact that indirect restorations are technique-sensitive, and success may often be contingent on operator skill and knowledge, as well as direct composite restoration. 3.3.. References. Akimoto N, Takamizu M, Momoi Y. 10-year clinical evaluation of a self-etching adhesive system. Oper Dent 2007; 32: 3-10. Baratieri LN, Ritter AV. Four-year clinical evaluation of posterior resin-based composite restorations placed using the total-etch technique. J Esthet Restor Dent 2001; 13: 50-57. Collins CJ, Bryant RW, Hodge KL. A clinical evaluation of posterior composite resin restorations: 8-year findings. J Dent 1998; 26: 311-317. Hickel R, Manhart J. Longevity of restorations in posterior teeth and reasons for failure. J Adhes Dent 2001; 3: 45-64.. 34.
(36) Jayasooriya PR, Pereira PNR, Nikaido T, Tagami J. Efficacy of a resin coating on bond strengths of resin cement to dentin. J Esthet Restor Dent 2003; 15: 105-113. Van Dijken JMV. Direct resin composite inlays/onlays: an 11 year follow-up. J Dent 2000; 28: 299-306.. 35.
(37) Acknowledgments This work was carried out at the Department of Operative Dentistry, Tokyo Dental College from 2006-2007. The present thesis is the result of the efforts of many people. I would like to express my deepest gratitude to all who have been involved with this study including those not directly mentioned below. It has been my privilege to work with all of them. I wish to express my sincere gratitude to Dr. Yoshito Hirai, Professor and Chairman of Department of Operative Dentistry, Tokyo Dental College, who provided me the opportunity and the access to facilities to undertake this study. I am deeply grateful to Dr. Atsushi Kameyama, Assistant Professor of the Department of Operative Dentistry, Tokyo Dental College, who instructed and supported me during my work. His guidance, knowledge and suggestions were essential to the outcome of my research. I wish to acknowledge my sincere gratitude to Mr. Katsumi Tadokoro of the Oral Health Science Center, Tokyo Dental College, who kindly supported me when using SEM. I also owe special thanks to Professors Yutaka Oda and Eiji Kawada of the Department of Dental Materials Science, Tokyo Dental College, for use of their measuring device. I would like to thank all staff members of the Department of Operative Dentistry, Tokyo Dental College, for always being friendly and kind. Finally I want to especially thank my parents, Mr. Mitsuru Oishi and Ms. Shoko Oishi, who constantly encouraged me to pursue my study and gave me all their love during my long six-year period of study at Tokyo Dental College.. November 30, 2007 Takumi Oishi. 36.
(38) Table 1-1 Representative contemporary adhesives categorized according to clinical application and chemical composition Adhesive. Manufacturer. Composition. pH. Three-step etch-and-rinse adhesives All-Bond 2. Bond-it. Clearfil Liner Bond. Imperva Fluorobond (FL Bond in USA). Bisco Inc., Etchant: 10% H3PO4 (All-etch) or Schaumburg, IL, 32% H3PO4 (Uni-etch) USA Primer A: NTG-GMA, acetone, ethanol, water Primer B: BPDM, photo-initiator, acetone Bonding (D/E resin): Bis-GMA, UDMA, HEMA Pentron Corporation, Wallingford, CT, USA. 5.7 (primers mixed). 7.5. Etchant: 37% H3PO4 Primer A: NTG-GMA, acetone Primer B: PMGDM, Bis-GMA, HEMA, photo-initiator, acetone Adhesive: Bis-GMA, HEMA, UDMA, HDDMA with amine accelerator, photo-initiator, BPO. Kuraray Medical Etchant: H3PO4 (K-etchant) Inc., Tokyo, SA primer: 5-NMSA, ethanol, Japan Photo Bond Catarist: MDP, HEMA, Bis-GMA, hydrophobic dimethacrylate, BPO, CQ Photo Bond Universal: DEPT, sodium benzen sulfinate, ethanol Shofu, Inc., Etchant: 7% H3PO4 (K-etchant) Kyoto, Japan Primer A: water, acetone, initiator 2.2 Primer B: 4-AET, 4-AETA, HEMA, UDMA, TEGDMA, photo-initiator. Two-step etch-and-rinse adhesives Adper Single Bond. 3M ESPE, St. Paul, USA. Etchant: 35% H3PO4 Adhesive: dimethacrylates, HEMA, polyalkenoid acid copolymer, silane treated colloidal silicam ethanol, water, photo-initiator. Bond-1. Pentron Corporation, Wallingford, CT, USA. Etchant: 37% H3PO4 Adhesive: PMGDM, HEMA, TMPTMA, initiators, acetone. Clearfil Photobond. Kuraray Medical Etchant: H3PO4 (K-etchant) Inc., Tokyo, Catalyst: MDP, HEMA, Bis-GMA, Japan hydrophobic dimethacrylate, BPO Universal: DEPT, sodium benzen sulfinate, ethanol.
(39) Table 1-1 (continued) Adhesive Manufacturer. Composition. Clearfil New Bond. Kuraray Medical Etchant: H3PO4 (K-etchant) Inc., Tokyo, Catalyst: MDP, HEMA, Bis-GMA, Japan hydrophobic dimethacrylate, BPO Universal: DEPT, sodium benzen sulfinate, ethanol. One-Step. Bisco Inc., Etchant: 32% H3PO4 (Uni-etch), Schaumburg, IL, 37%H3PO4 (Etch-37) USA Adhesive: BPDM, Bis-GMA, HEMA, acetone, photo-initiator. Prime&Bond NT. Dentsply De Trey, Konstanz, Germany. pH. Etchant: H3PO4 Adhesive: PENTA, TEGDMA, BisGMA, cetylamine hydrofluoride, acetone, nanofiller, resin R5-62-1, T-resin, D-resin, CQ. Two-step self-etch adhesives Clearfil Liner Bond II. Kuraray Medical Primer A: Phenyl-P, 5-NMSA, CQ, Mixed primer: 1.4 Inc, Tokyo, Japan ethanol Primer B: HEMA, water LB BOND: MDP, HEMA, hydrophobic dimethacrylate, CQ, silanated colloidal silica. Clearfil Liner Bond II Σ. Kuraray Medical Primer A: MDP, HEMA, hydrophilic Mixed primer: 2.8 Inc, Tokyo, Japan dimethacrylate, CQ, DEPT, photoinitiator, water Primer B: HEMA, hydriphilic dimethacrylate, water Bond A: MDP, HEMA, hydrophobic dimethacrylate, CQ, silanated colloidal silica Bond B: HEMA, Bis-GMA, hydrophobic dimethacrylate, BPO, DEPT, CQ, silanated colloidal silica. Clearfil Megabond. Kuraray Medical Primer: MDP, HEMA, hydrophilic 2.0 Inc, Tokyo, Japan dimethacrylate, photo-initiators, silanated colloidal silica Bond: MDP, HEMA, Bis-GMA, hydrophobic dimethacrylate, photo-initiators, silanated colloidal. Clearfil Megabond FA Kuraray Medical Primer: MDP, MDPB, HEMA, 2.0 Inc, Tokyo, Japan hydrophilic dimethacrylate, photoinitiators, silanated colloidal silica Bond: MDP, HEMA, Bis-GMA, hydrophobic dimethacrylate, photo-initiators, silanated colloidal silica, NaF.
(40) Table 1-1 (continued) Adhesive Manufacturer. Composition. pH. Unifil Bond. GC, Tokyo, Japan. Primer: 4-MET, HEMA, ethanol, 2.0 water, CQ Bonding: UDMA, HEMA, DMA, CQ, silica. Tokuso Mac Bond II. Tokuyama Dental, Tokyo, Japan. Self-etching primer (a+b): MAC10, methacryloylalkyl acid phosphate, water, acetone Bonding: MAC-10, HEMA, BisGMA, TEGDMA, CQ. One-step self-etch adhesives Absolute. Dentsply Sankin Methacrylate ester, fluoride Kogyo, Ohtawara, compound, anhydrous silicic acid, Japan acetone. Adper Prompt L-Pop 3M ESPE, St. Paul, USA. Red cushion: Methacrylic phosphates, Bis-GMA, photoinitiator Yellow cussion: Water, HEMA, polyalkenoic acid polymer. AQ Bond Plus. San Medical, Liquid: water, acetone, 4-META, Moriyama, Shiga, UDMA, monomethacrylates, photoJapan initiator, stabilizer Eponge: sodium p-toluensulfinate. Clearfil S3 Bond. Kuraray Medical, MDP, Bis-GMA, photo-initiators, Tokyo, Japan ethanol, water, silanated colloidal silica. G-Bond. GC, Tokyo, Japan. iBond. Heraeus Kulzer, UDMA, 4-META, gluraraldehyde, Hanau, Germany acetone, water, photo-initiators, stabilizers. One-up Bond F Plus. Tokuyama Dental, Tokyo, Japan. Reactomer Bond. Shofu Inc, Kyoto, Bond A: F-PRG filler, fluoroJapan alumino-silicate glass, water, acetone, initiator. 4-MET, phosphoric ester monomer, UDMA, TEGDMA, acetone, water, stabilizer, silica filler, water, photo-initiator. Bonding agent A: MAC-10, photo- 0.7 initiator, methacryloylalkyl acid phosphate, multi-functional methacrylic monomer Bonding agent B: MMA, HEMA, 7.7 (A+B: 1.2) water, F-deliverable micro-filler (fluoro-alumino-silicate glass), photo-initiator 2.6.
(41) Table 1-1 (continued) Adhesive Manufacturer. Composition. pH. Bond B: F-PRG filler, fluoroalumino-silicate glass, water, acetone, initiator Xeno CF II. Dentsply Sankin Bottle A: HEMA, ethanol, water, Kogyo, Ohtawata, aerosil, stabilizers Japan Bottle B: Pyro-EMA, PEM-F, UDMA, CQ, BHT, ethyl-4dimethylaminobenzoate (co-. <1.
(42) Table 2-1 Materials used in this study Material. Manufacturer. Components/Shade (Lot No.). Principle ingredients. Procedure. pH. GC, Tokyo, Japan. Primer (0507201). HEMA, Ethanol, 4-MET. Apply primer (20 sec.), air dry, apply bonding agent, light cure (10 sec.). 2.0. Bonding agent. UDMA, HEMA, CQ. Etchant (6KT). Phosphoric acid. 《 Adhesive》 UniFil Bond. Adper Single Bond. 3M ESPE, St Paul, MN, USA. Adhesive (6KP). -0.2 (Koase et al.) Apply etchant (15 sec.), rinse with water spray (10 sec.), gentle air dry (1 sec.), HEMA, water, ethanol, amines, apply two consecutive coats 4.3 (Proenca et al.) bis-GMA, DMA, copolymer of of the adhesive with a fully polyacrylic and polyitaconic saturated brush tip, gentle acids, CQ air dry (5 sec.), light cure (10 sec.). 《 Flowable composite》 UniFil Flow. GC, Tokyo, Japan. A3 shade (0610171). Fluoro-Alumino Silicate Glass, Apply with brush-tip, light Di-2-Methacryloyloxyethyl cure (20 sec.) 2,2,4-trimethylhexamethylene dicarbamate, Silica, TEGDMA. Self-etching primer A (0610071). water, 4-MET, ethanol, methacryloyloxyesther. 1.5. Self-etching primer B (0610071). ethanol, catalyst. 6.0. Paste A/B (clear shade) (0610133). fluoro-alumino silicate glass, HEMA, UDMA, methacryloyloxyester, silica, catalyst. Composite primer. 2 Hydroxyethyl Methacrylate, Di-2- Methacryloyloxyethyl, 2,2,4-trimethylhexamethylene dicarbamate. Coat composite primer to the bonded Gradia surface with brush-tip, light cure (20 sec.). Translucent shade. Alumino-silicate glass, Amorphous Precipitated Silica, Di-2-Methacryloyloxyethyl 2,2,4-trimethylhexamethylene dicarbamate, Neopentylglycol dimethacrylate. Pre-cure (20 sec. for each side) with New Light VL-2, final cure (Triad 2, Dentsply International; 5 min. each side), sandblast the bonded surface with 50 μm alumina.. 《 Resin adhesive luting cement》 Linkmax. GC, Tokyo, Japan. 《 Indirect composite》 Gradia. GC, Tokyo, Japan. 2.0 (A+B ).
(43) Table 2-2 µ-TBS (Mean ± S.D.) for all tested groups. UniFil Bond. Mean (MPa). SD. PTF/n. Statistics. Regular. 25.6. 10.8. 1/19. b. Superfine. 38.1. 18.5. 0/19. a. 20.1. 13.6. 4/17. bc. Superfine. 10.7. 13.4. 16/28. cd. Regular. 16.4. 8.9. 1/19. cd. Superfine. 19.9. 11.4. 2/20. c. Adper Single Bond Regular. Non-coated (Control). PTF: pre-tested failure, n : number of specimen Same letters represent no statistically significant difference (Tukey-Kramer test; p <0.05).
(44) Fig. 1-1 Classification of contemporary adhesives according to Van Meerbeek et al (2005)..
(45) Fig. 1-2. Schematic overview of the interaction of different self-etch adhesives with dentin. (From De Munck et al 2005.).
(46) Fig. 1-3 Clinical factors influencing resin-dentin bonding..
(47) a. b. c. PMMA cube. e. f. 1.4 x 0.7 mm Fig. 2-1. Resin coating. d. Gradia disc. g. CHS: 1 mm/min. Schematic diagram of specimen preparation for micro-tensile bond strength..
(48) Non-coated. Adper Single Bond. Unifil Bond. 0% Regular. Superfine. Regular. 20%. 40%. 60%. 80%. 100%. R R/A A/R I D. Superfine. Regular. Superfine. Fig. 2-2 Distribution (as percentage) of failure modes according to stereomicroscopic observation. R: 100% cohesive in resin, R/A: Mixed, mainly cohesive in resin and partially at adhesive interface, A/R: Mixed, mainly at adhesive interface and partially cohesive in resin, I: 100% at adhesive interface, D: 100% cohesive in dentin..
(49) a. b RC. HL. RC. ?. CM HL. ?. Fig. 2-3 Representative SEM images of fractured surfaces on the dentin side after micro-tensile bond strength test. (a) UniFil Bond/regular, 21.8 MPa, (b) UniFil Bond/superfine, 43.2 MPa. Mixed failure of adhesive interfacial area failure and cohesive failure in coated resin are apparent. Almost all dentinal tubules are plugged with coated material (pointer). RC: Resin cement, CA: coated material, HL: hybrid layer..
(50) a. b. ? ?. Fig. 2-4. ?. Representative SEM images of the fractured surfaces on the dentin side after micro-tensile bond strength test. (a) Single Bond/regular, 23.3 MPa, (b) Single Bond/superfine, 11.2 MPa. Failure in adhesive interfacial area is shown in all parts. Opened dentin tubules are clearly observed. Arrow: scratches caused by preparation with diamond bur..
(51) a. b. ?. Fig. 2-5. ?. Representative SEM images of the fractured surfaces on the dentin side after micro-tensile bond strength test. (a) Non-coated/regular, 15.7 MPa, (b) Non-coated/superfine, 20.5 MPa. Mixed failure of adhesive interfacial area failure and cohesive failure in resin cement are apparent. Almost all dentinal tubules were plugged with resin cement (pointer). Arrow: scratches caused by bur-grinding..
(52) Appendix Oral presentation at the 55th Annual Meeting of Japanese Association for Dental Research (Tsurumi University Memorial Hall, November 18th, 2007).
(53) Appendix : Oral presentation at the 55th Annual Meeting of Japanese Association for Dental Research (Tsurumi University Memorial Hall, November 18th, 2007).
(54)
図

関連したドキュメント
Standard domino tableaux have already been considered by many authors [33], [6], [34], [8], [1], but, to the best of our knowledge, the expression of the
In this work we apply the theory of disconjugate or non-oscillatory three- , four-, and n-term linear recurrence relations on the real line to equivalent problems in number
This year, the world mathematical community recalls the memory of Abraham Robinson (1918–1984), an outstanding scientist whose contributions to delta-wing theory and model theory
If condition (2) holds then no line intersects all the segments AB, BC, DE, EA (if such line exists then it also intersects the segment CD by condition (2) which is impossible due
The inclusion of the cell shedding mechanism leads to modification of the boundary conditions employed in the model of Ward and King (199910) and it will be
2 Combining the lemma 5.4 with the main theorem of [SW1], we immediately obtain the following corollary.. Corollary 5.5 Let l > 3 be
We reduce the dynamical three-dimensional problem for a prismatic shell to the two-dimensional one, prove the existence and unique- ness of the solution of the corresponding
Altering one knot value, curve points move on well-defined paths, the limit of which can be computed if the knot value tends to infinity.. Symmetric alteration of two knot values