INTRODUCTION
The origin of a narrow duct segment distal to the enlarged common bile duct in congenital choledochal cysts is controversial. In 1936, Yotuyanagi described this duct system and termed it “ductus pancreaticobiliosis” based on the anatomical findings of autopsy cases1). Bab-bitt detected the narrow duct system using direct cholangiography in 3 children with con-genital cystic dilatation of the bile duct (CCBD,
Alonso-Lej Type I3)) and described the narrow duct as a long common channel, defining it as an “anomalous arrangement of the pancreatico-biliary ductal system”2). Both of those authors suspected that the narrow duct system was a pre-disposing factor in the occurrence of CCBD, and subsequently this hypothesis became well known throughout the world.
Since Babbitt’s report, further investigations of pancreaticobiliary maljunction (PBM) have been done. The Japanese Study Group on Pan-creaticobiliary Maljunction presented extramur-al location of the union of the terminextramur-al bile
Variations of the Union between the Terminal Bile Duct
and the Pancreatic Duct in Patients
with Pancreaticobiliary Maljunction
Hideki F
UJII1) 1)Department of Surgery, School of Medicine, Yamanashi University, Tamaho, Nakakoma, Yamanashi, 409-3898, Japan
Abstract: Background and Purpose:
Pancreaticobiliary maljunction (PBM) is an anomaly with an extramural location of the union between the bile duct and the pancreatic duct system in the duodenum, and is probably caused by disarrangement of the embryonic connection between the two duct systems that presents varied clini-cal manifestations. The aim of this study was to analyze and categorize various patterns of connection between the two duct systems in PBM patients in order to improve the precision of the diagnosis of PBM and to establish safe surgical procedures to treat it.
Materials and Methods:
We made group classifications of the patterns of connection between the two duct systems in 226 PBM patients based on radiologic or/and anatomical examinations.
Results:
The 226 cases of PBM were divided into three groups: Group A, 2 patients with a complicated con-nection pattern, Group B, 176 patients with a notch or a small duct segment distal to the terminal bile duct, Group C, 48 patients without a notch or the segment at the terminal bile duct.
Conclusion:
In Group A, the terminal bile duct was probably connected to one of the multi-branched main ducts of the ventral pancreas, while in Group B, it was probably connected to a second branch of the ventral pancreas, and in Group C, directly to the main pancreatic duct.
Key words: pancreaticobiliary maljunction, choledochal cyst, embryology
Received October 28, 2003 Accepted October 29, 2003
duct and the pancreatic duct in the duodenum as a definition of PBM4). However, how PBM arises during embryogenesis remains unclear. Recently we proposed an hypothesis, based on radiological and anatomical analyses of PBM, that the narrow duct system was neither a nar-rowed bile duct nor a common channel of the two duct systems, but was rather part of the pan-creatic duct system5). That is, the development of PBM during embryogenesis is probably caused by disarrangement of the embryonic connection between the biliary and pancreatic ducts in an early period of gestation5).
However, this connection may occur at vari-ous locations of the duct system of the ventral pancreas5), and moreover, PBM is often accom-panied by other malformations of the hepatobil-iary system and pancreas such as CCBD2), con-genital stricture of the intrahepatic bile duct6) and pancreas divisum7,8). Consequently, the con-nection pattern between the two duct systems may be extremely complicated, and making a precise diagnosis of PBM will continue to be very difficult in PBM patients with a short com-mon duct5) if the embryo genetic etiology of PBM is not clarified.
The aim of this study was to analyze the anatomical variations in the location of the union and in the patterns of connection of the terminal bile duct with the pancreatic duct sys-tem in patients with PBM, in order to improve the precision of the diagnosis of PBM and to establish safe surgical procedures. We believe that making a precise diagnosis of PBM, which carries a high risk of bile duct cancer, is impor-tant for preventing the development of bile duct cancer9,10).
PATIENTS ANDMETHODS
Patients
Of 2,613 patients who underwent ERCP in our institute, 226 had PBM. The 226 PBM patients consisted of 70 males and 156 females, 158 of whom had benign biliary or/and pancre-atic diseases and 68 who had a malignant tumor of the biliary system, while 146 patients had CCBD and 80 did not. The age of the 226 patients ranged from 6 to 81 years and the mean age of the patients with benign biliary dis-ease was 60 ± 11 years in 54 males and 53 ± 13 years in 104 females. The mean age of the PBM patients with biliary malignancy was 66 ± 13 years in 16 males and 63 ± 12 years in 52 females.
DIAGNOSTICCRITERIA ANDPBM DETECTION The Japanese Study Group on Pancreaticobil-iary Maljunction has defined PBM as a congeni-tal anomaly in which the junction of the pancre-atic and biliary ducts is radiologically and/or anatomically detected outside of the duodenal wall (extramural location)[4]. We made a diag-nosis of PBM by means of ERCP, PTC, and/or anatomical confirmation based on operative findings during transduodenal papilloplasty or examination of pancreatoduodenectomized specimens or autopsy materials. Radiological detection of the extramural location of the union of the two ducts in the duodenum was performed according to the methods described previously5).
RESULTS
The 226 PBM patients were classified into three groups according to whether or not they had the following characteristics: 1) a
compli-cated connection of the terminal bile duct or the cystic dilatation of the bile duct with the pancreatic duct system, 2) evidence of a notch or a small duct distal to the bile duct (narrow duct segment11)), and 3) no evidence of a notch or small duct at the union of the bile duct with the ventral pancreas duct on direct cholan-giopancreatograms. Here “notch” means a v-shaped indentation on the terminal bile duct near the union of the bile duct and the main pancreatic duct seen on the cholangiopancre-atogram, and “a small duct” means a much nar-rower duct distal to the terminal bile duct or to the biliary cyst. PBM was frequently associated with pancreas divisum, especially partial pan-creas divisum7)in which there was only commu-nication between a small branch of the ventral pancreas and one of the dorsal pancreas. We
encountered no case in which there was a union of the bile duct and the dorsal pancreatic duct.
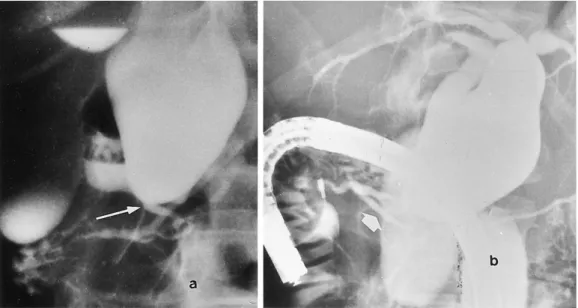
1. Group A: PBM patients in whom the con-nection of the terminal bile duct (or the bottom of the biliary cyst) with the pancre-atic duct showed a complicated pattern. Two of the 226 patients were classified into this group. In these patients, ERCP revealed multi-branching of the main pancreatic duct of the ventral pancreas and communication of the biliary cyst with one of the branches, as shown in Fig. 1a and 1b.
2. Group B: PBM patients in whom a notch or a small duct distal to the terminal bile duct was detected at the point of union between the two duct systems.
Of the 226 patients, 176 were classified into this group. Direct cholangiograms of patients in
Fig. 1. ERCP of a 37-year-old woman with Group A PBM, CCBD, pancreas divisum, and a biliary cyst, discov-ered by AUS in a mass survey screening.
a) The terminal bile duct can be seen to join with a pancreatic duct (long thin arrow). However, the main pancreatic duct branches away into at least three branches, and one of them is connected with the biliary cyst at the bottom of the cyst.
b) The dorsal pancreatic duct (arrow) is visualized by the flow of contrast medium through the major papilla. These images show multi-branching of the main duct of the ventral pancreas and the con-nection between the ventral and the dorsal pancreatic duct (partial pancreas divisum).
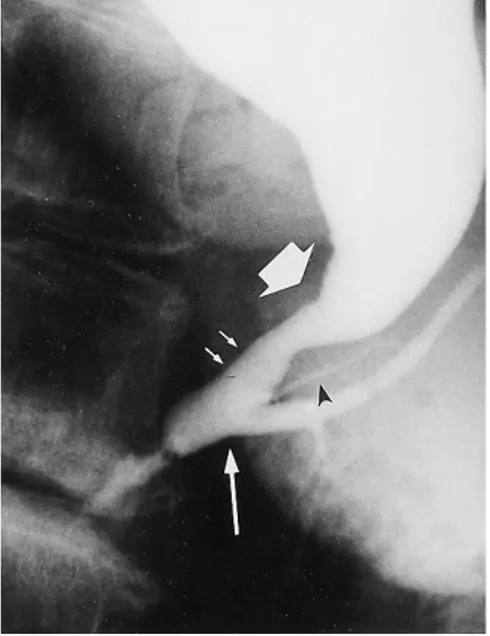
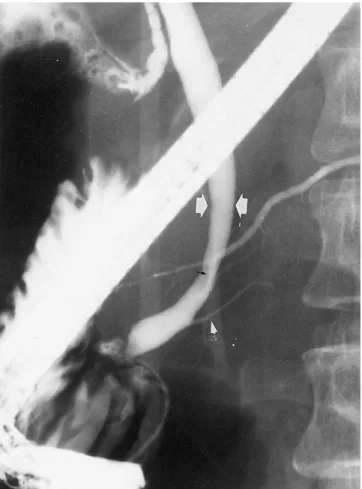
this group showed a notch or a small duct seg-ment in the distal portion of the terminal bile duct (or the biliary cyst). In Fig. 2, a T-tube cholangio-pancreatogram shows a notch in the distal portion of the terminal bile duct, and this finding is thought to imply that a second branch of the pancreatic duct is interposed between the bile duct and the main pancreatic duct. Figure 3 reveals a small duct distal to the biliary cyst and a smaller pancreatic duct that arises from the small duct (narrow duct seg-ment11)). Figure 4 shows the ERCP image after
resection of a biliary cyst in a case of CCBD. The main pancreatic duct appears to enter a large U-shaped duct, which seems to be the intrapancreatic portion of the common bile duct. But the U-shaped duct is considered to correspond to the “common duct” which occurs in PBM patients and consists of a narrow duct segment and part of the main pancreatic duct. This type of connection is considered to indi-cate that the bile duct is anatomically joined with the main duct of the ventral pancreas, accompanied by an interposition of the second or third branch of the ventral pancreatic duct between the two ducts.
3. Group C: PBM patients in whom a notch or Fig. 2. T-tube cholangiogram of a 31-year-old
woman with Group B PBM, after cholecystectomy.
The terminal bile duct is seen to join with a small radicle (2 small thin arrows) arising from the main pancre-atic duct (arrow) near the duodenal wall and a notch is formed in the distal portion of the bile duct. The terminal bile duct is seen to be suddenly reduced in diameter, showing an irreg-ular shape at the distal end and con-necting with the small radicle arising from the main pancreatic duct. This small radicle was a second branch of the ventral pancreatic duct.
Fig. 3. ERCP of a 65-year-old woman with Group B PBM, CCBD and gallblad-der cancer.
A narrowed duct segment (2 small thin arrows) distal to the biliary cyst ca be seen. This segment is joined with the main pancreatic duct (long thin arrow). A small radicle (arrow-head) arising from the narrow duct segment can be seen. The narrowed duct segment is thought to be a sec-ond branch of the ventral pancreatic duct.
a small duct distal to the terminal bile duct was not detected at the union of the two ducts.
Group C consisted of 48 patients with PBM. An ERCP (Fig. 5) of a representative PBM patient in this group demonstrated that the ter-minal bile duct was joined with the main pan-creatic duct near the duodenal wall, without a notch or a small duct on the terminal bile duct. Figure 6 shows that the terminal bile duct was
Fig. 4. ERCP after resection of the bile duct cyst in a 20-year-old woman with Group B PBM and CCBD.
The main pancreatic duct (long thin arrow) enters to a U-shaped large duct, which seems to be the intrapancreatic portion of the common bile duct at the point indicated by an asterisk, of which the top (indicated by an arrow) corre-sponds to the proximal end of the nar-row duct segment distal to the resected biliary cyst. Small pancreatic duct radi-cles (arrowhead) arising from the U-shaped large duct can also be seen. Although the diameter of the U-shaped large duct and the main pancreatic duct are different, the duct from the major papilla (large arrow) to the tail of the pancreas corresponded to the main pancreatic duct, and the segment of the U-shaped large duct from the asterisk to the arrow was the second branch of the pancreatic duct.
Fig. 5. ERCP of a 41-year-old woman with Group C PBM and acute cholecystitis. The terminal bile duct is joined to the main pancreatic duct near the duode-nal wall (arrow) without a notch or a small duct.
Fig. 6. Operative cholangiogram of a 7-year-old boy with Group C PBM, CCBD and bile duct stone.
The terminal bile duct is joined (large arrow) to the main pancreatic duct far from the duodenal wall without a notch or a small duct.
Fig. 7. ERCP of a 55-year-old woman with Group C PBM, partial pancreas divisum and gallbladder cancer.
The whole extrahepatic bile duct, part of the intrahepatic ducts, and the dorsal pancreatic duct (via the small duct indicated by a small arrow) were revealed by the flow of contrast medium through the major papilla. The terminal bile duct was directly joined (arrow) with the proximal end of the main duct of the ventral pancreas and a small pan-creatic radicle (the high density line is indicated by a small arrow) was connected with the large duct from the major papilla (ventral pancreatic duct) and the dorsal pancreatic duct from the minor papilla to the pancreatic tail (partial pancreas divisum). Small pancreatic radicles (arrowhead) arose from the large duct from the major papilla, which is thought to be the main duct of the ventral pancreas.
joined with the main pancreatic duct far from the duodenal wall without a notch or a small duct segment. Figure 7 shows that the extrahep-atic bile duct and the dorsal pancreextrahep-atic duct via a small duct arising from the main duct of the ventral pancreas (partial pancreas divisum7,8)). In this case, the terminal bile duct was consid-ered to be joined directly with the proximal end of the main duct of the ventral pancreas.
DISCUSSION
Extramural location of the union of the ter-minal bile duct and the pancreatic duct in the duodenum was not recognized in the past as an anomaly in the pancreaticobiliary ductal system, but was rather thought to be a normal variations9,12–14). However, in several reports that described detailed analyses of the location of the junction of the terminal bile duct and the pancreatic duct based on anatomical and/or radiological examinations, a long common channel15)or extramural location of the union in the duodenum15–17)was not found in normal cases, but was found in cases of CCBD, congeni-tal biliary atresia (CBA)18)or acute pancreati-tis12,19).
Since Babbitt’s key report about PBM2), our knowledge about “a long common channel” has increased, and diagnostic criteria for PBM were presented by the Japanese Study Group on Pan-creaticobiliary Maljunction4). However, the mechanism of embryonic development of PBM was not clarified ay that time. We hope that our hypothesis about the mechanism of PBM devel-opment will aid progress in making a precise diagnosis of PBM and the establishment of safe surgical procedures for PBM. In this report, we presented various cholangiopancreatograms of PBM patients with various locations or/and anomalous connections due to an embryonic
disarrangement between the bile duct and the pancreatic duct, and investigated the essential patterns of the disarrangement with the aim of establishing safe and appropriate surgical pro-cedures for this disease. Moreover, a notch or a small duct segment was noted to be a key point of detecting PBM. We showed that the anatomi-cal location of the union could exist at any site in the duct system of the ventral pancreas. In our series, 136 of the 226 PBM patients had a short common duct less than 1 cm in length, and these 136 patients consisted of 113 patients in Group B and 23 in Group C. The remaining 90 of the 226 patients had a long common duct over 1 cm in length, and they consisted of the 2 patients in Group A, 63 patients in Group B and 25 patients in Group C. A short common duct was apparently formed due to the location of the union near the duodenal wall in Group C patients and also in patients with a notch (not a small duct) in Group B. On the other hand, a long common duct was seen in Group B patients with a small duct segment and in Group C patients with the location of the union far from the duodenal wall, and also in Group A patients. Figure 8 shows a schematic diagram showing the possible anatomical points of the union.
Clinical manifestations in PBM patients, such as acute pancreatitis12,19), intermittent abdomi-nal pain, obstructive jaundice, acute cholangitis, primary bile duct stones20) and bile duct can-cer21,22)did not correlate with the presence of a long or a short common duct, with accompany-ing CCBD5) or the connection patterns. These clinical features do not correlate with the length of the common duct in PBM patients, so it is dif-ficult to detect the extramural location of the union in the duodenum, especially in patients with a short common duct.
and the development of gallbladder cancer, PBM was found in 45 of 112 patients with gall-bladder cancer treated in our institute during the study period. Since PBM is considered to be a high risk condition for the development of gallbladder cancer23), we make it a rule that PBM patients receive cholecystectomy as soon as possible even if the patients have no clinical manifestations, in order to prevent the develop-ment of gallbladder cancer21–23). Moreover, since CCBD with PBM is also known to be associated with a high-risk condition for the development of bile duct cancer, preventive surgery is recom-mended when the disease is discovered. It is well known that an extirpation of the biliary cyst is the most appropriate procedure, but details of the optimal approach for the intrapancreatic portion of the biliary cyst, as well as those for the proximal portion of the cyst, remain contro-versial. It is important to establish a practical and safe procedure for treatment of the anom-aly with the goals of avoiding intraoperative
injury of the main pancreatic duct and prevent-ing the development of cancer originatprevent-ing from a remnant cyst wall. The classification of the patterns of connection between the bile duct and the pancreatic duct into the groups described here should be helpful for the opti-mization of the surgical approach. A complete resection of the bile duct or the biliary cyst is possible only for patients with a small duct seg-ment in Groups A and B. Resection of the ter-minal bile duct or the biliary cyst in patients with a notch in Group B and in patients in Group C must be performed in a manner that retains part of the terminal bile duct in order to avoid injury of the main pancreatic duct.
REFERENCES
1) Yotuyanagi S. Contributions to the etiology and pathogeny of idiopathic cystic dilatation of the common bile duct with report of three cases: a new etiological theory based on supposed unequal epithelial proliferation at the stage of Fig. 8. Schematic diagram showing possible anatomical points of the union between the terminal bile
duct and the ventral pancreatic duct, indicated by numbers corresponding to those of Figs. 1–7. D: a small pancreatic duct connecting the dorsal and the ventral pancreatic duct in partial
pan-creas divisum.
the physiological epithelial occlusion of the primitive choledochus. GANN 30: 601–650, 1936.
2) Babbitt DP. Congenital choledochal cyst: new eti-ological concept based on anomalous relation-ships of common bile duct and pancreatic duct. Ann Radiol 12: 231–241, 1969.
3) Alonso-Lej F, Rever WB, Pessagno DJ. Congenital choledochal cyst with a report of two and analy-sis of 94 cases. Int Abstr Surg 108: 1–23, 1959. 4) The Japanese Study Group on Pancreaticobiliary
Maljunction: Diagnostic criteria of pancreatico-biliary maljunction. J Hepatopancreatico-biliary Pancreat Surg 1: 219–221, 1994.
5) Matsumoto Y, Fujii H, Itakura J, Mogaki M, Mat-suda M, et al. Pancreaticobiliary Maljunction: eti-ologic concepts based on radieti-ologic aspects. Gas-trointest Endosc 53: 614–619, 2001.
6) Matsumoto Y, Fujii H, Yoshioka M, Sekikawa T, Wada T, et al. Biliary strictures as a cause of pri-mary intrahepatic bile duct stone. World J Surg 10: 867–875, 1986.
7) Douglas CW, Michael VS. Partial pancreas divi-sum. Cleveland Clin J Med 54: 33–37, 1988. 8) Itakura J, Fujii H, Matsumoto Y, Suda K.
Clinico-pathological studies of anomalous arrangement of the pancreaticobiliary ductal system with pan-creas divisum. J Hepatobiliary Pancreat Surg 1: 240–246, 1994.
9) Kimura K, Ohto M, Saisho H, Unogawa T, Tsuchiya Y, et al. Association of gallbladder carci-noma and acarci-nomalous pancreaticobiliary ductal union. Gastroenterol 89: 1258–1265, 1985. 10) Kinoshita H, Nagata E, Hirohashi K, Sakai K,
Kobayoshi Y. Carcinoma of the gallbladder with an anomalous connection between the chole-dochus and the pancreatic duct: report of 10 cases and review of the literature in Japan. Can-cer 54: 762–769, 1984.
11) Suda K, Matsumoto Y, Miyano T. Narrow duct segment distal to choledochal cyst. Am J Gas-troenterol 86: 1259–1263, 1991.
12) Hicken NF, McAllister AJ. Is the reflux of bile into the pancreatic ducts a normal or abnormal physiologic process? Am J Surg 89: 781–786, 1952.
13) Dowdy GS, Waldron GW, Brown WG. Surgical anatomy of the pancreatobiliary ductal system. Arch Surg 84: 93–110, 1962.
14) Misra SP, Gulati P, Thorat VK, VIJ JC, Anand BS. Pancreaticobiliary ductal union in biliary dis-eases; An endoscopic retrograde cholangiopan-creatographic study. Gastroenterol 96: 907–912, 1989
15) Jones GM, Caylor HD. Anomalous termination of common duct Am J Surg 93: 122–123, 1957. 16) Hand BH. An anatomical study of
choledo-choduodenal area. British J Surg 50: 486–494, 1963.
17) Suda K, Miyano T, Hashimato K. The choledo-cho— pancreatico-ductal junction in infantile obstructive jaundice disease. Acta Pathol Jpn 30: 187–194, 1980.
18) Arima E, Akita H. Congenital biliary tract dila-tion and anomalous juncdila-tion of the pancreatico-biliary ductal system J Pediatr Surg 14: 9–15, 1979.
19) Schweiger P, Schweiger M. Pancreaticobiliary long common channel syndrome and congenital anomalous dilatation of the choledochal duct − study of 46 patients. Eur J Pediatr Surg 3: 15–21, 1993.
20) Matsumoto Y, Uchida K, Nakase A, Honjo I. Con-genital cystic dilatation of the common bile duct as a cause of primary bile duct stone. Am J Surg 134: 346–352, 1977.
21) Tanno S, Obara T, Fujii T, Mizukami Y, Shuda R, et al. Proliferative potential and K-ras mutation in epithelial hyperplasia of the gallbladder in patient with anomalous pancreaticobiliary ductal union. Cancer 83: 267–275, 1998.
22) Hanada K, Itoh M, Fujii K, Tsuchida A, Ooishi H, et al. K-ras and P53 mutations in Stage Ⅰ gall-bladder carcinoma with an anomalous junction of the pancreaticobiliary duct. Cancer 77: 452–458, 1996.
23) Matsumoto Y, Fujii H, Itakura J, Matsuda M, Suda K. Recent advances in pancreaticobiliary maljunction: clinical significance and carcino-genesis. J Hepatobiliary Pancreat Surg 9: 45–54, 2002.