つくばリポジトリ SR 7 1 2364
全文
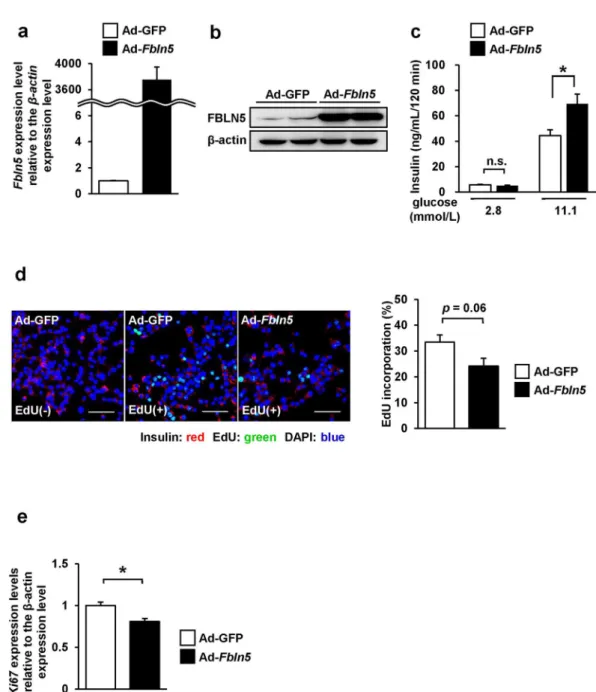
図
関連したドキュメント
During land plant evolution, stem cells diverged in the gametophyte generation to form different types of body parts, including the protonema and rhizoid filaments, leafy-shoot
Here, cell surface localization of MT1-MMP and activation of MMP-2 were clearly induced in mesothelioma cells even when expression of integrin 1 was substantially abolished..
However, VPA prevented the morphological changes characteristic for activation and inhibited the expres- sion of collagen type 1 α 1 (COL1A1) and TGF- β 1 in activated LI90 cells
Determination of the Levels of Phosphorylated MAPK and GTP-bound Rac1—J774[SR-BI] cells or HEK293 cells forcedly expressing rat SR-BI and FLAG-tagged human GULP were incubated in
They proved that if Y is a (real or complex) rearrangement-invariant nonatomic function space on [0, 1] isometric to L p [0, 1] for some 1 ≤ p < ∞ then the isometric isomorphism
(Place a 0{cell in the center and form two 1{cells oriented towards the center.) For the relative case we use the relative version of the Framed Graph Theorem to construct a
By con- structing a single cone P in the product space C[0, 1] × C[0, 1] and applying fixed point theorem in cones, we establish the existence of positive solutions for a system
The techniques employed in this paper are also applicable to Toeplitz matrices generated by rational symbols b and to the condition numbers associated with l p norms (1 p 1 )