INTRODUCTION
Cerebral palsy (CP) is primarily a disorder of movement and posture. CP is the most common motor disability in childhood. It is defined as a group of non - progressive, but sometimes changing, motor impairment syndromes secondary to lesions of the affected brain arising in the early stages of its development (1).
CP is a common problem, the worldwide incidence being 2 to 2.5 per 1,000 live births (2). The etiology of CP is very diverse and multifactorial. The causes are congenital, genetic, inflammatory, infectious, anoxic, traumatic and metabolic (3). The Gross Motor Functional Classification System (GMFCS) describes the func-tional characteristics in five levels, from I to V. Level I being the mildest in the following age groups : up to 2 yrs, 2!4 yrs, 4 !6 years and between 6 to 12 years. For each level, separate de-scriptions are provided (4).
Although there have been no general studies of life expec-tancy in a population with CP, most children affected by CP live between 30 and 70 years, depending on the severity of the condi-tion. Most children with even the mildest form of CP tend to have slightly shorter life spans than the general population (5). Individuals with CP have a lower life expectancy than the general population, with one study of a Californian population demonstrating a mor-tality of 90 per 1,000 (6). Respiratory diseases are often considered the main cause of death in CP, but there have been a few studies of cause - specific mortality. In a recent investigation of individuals with developmental disability in London, Hollins and co - workers (1998) reported that 52% of the deaths were due to respiratory
dis-eases. Plioplys and co - workers (1998) found 77% of the deaths to be due to pneumonia in their population (mostly children) with very severe neurological disabilities (7).
Several studies have been published regarding the cause of death in children with CP. The risk factor of mortality in CP at Dr. Soetomo Hospital, Indonesia has never been investigated.
MATERIALS AND METHODS
Study and designAn observational analytic study was conducted using medical records of hospitalized CP patients in the pediatric ward at Dr. Soetomo Hospital, Surabaya, Indonesia, from January 2014 to December 2016. The inclusion criteria was all of the cerebral palsy patients that were hospitalized in Dr. Soetomo Hospital from 6 months to 14 year of age on the basis the motor disability caused by damage on central nerve system during the period from preg-nancy to the period of brain development (5 year of age). The patients were excluded if they suffered from severe mental retarda-tion without motoric problem, spinal disorder/peripheral nerve disorder, and neuromuscular disease and had incomplete data. In-formation collected included the demographic data of the patients, admission, diagnosis and outcomes.
Mortality information was obtained from annual computer and matched against the subjects with CP on the basis of name, date of birth, type of disability, degree of disability, nutritional status and the outcomes. We identified 12 patients who died during the study period. Causes of death are given on the computer tapes in the form of ICD- 9 codes.
Statistics
All data was analyzed using IBM SPSS Statistics 21 software. Risk factors were counted using logistic regression with P values
ORIGINAL
Risk Factor of Mortality in Indonesian Children with Cerebral
Palsy
Prastiya Indra Gunawan1, Risky Vitria Prasetyo1, Mira Irmawati1, Retno Asih Setyoningrum1, Darto Saharso1, and
Erny Prasetyo2
1
Department of Child Health, Airlangga University College of Medicine, Dr Soetomo Hospital, Surabaya, Indonesia2Department of Child
Health, Wijaya Kusuma College of Medicine, Surabaya, Indonesia
Abstract
Objective : Individuals with CP have a lower life expectancy than the general population. The objective of the study is to investigate the risk factor of mortality in Indonesian children with CP. Methods : An observational analytic study was conducted using medical records at pediatric ward Dr. Soetomo Hospital, Surabaya, Indonesia, from January 2014 to December 2016. Inclusion criteria was all of CP patients in that were hospitalized from 6 months to 14 year of age. Mortality information was obtained from annual computer and matched against the subjects with CP on the basis of name, date of birth, type of disability, degree of disability, nutritional status and the outcomes. Risk factors were counted using logistic regression. Result : Fifty five children were enrolled. The outcome revaled 12 patients (21.8%%) were death. Pneumonia was the most common underlying disease cause of death (OR=5.185 ; 95%% CI 1.249 to 21.520 ; P!0.007). Other risk factors of mortality that significant were acute kidney injury (AKI) (OR=3.333 ; 95%% CI 1.317 to 8.436 ; P!0.03). and Gross Motor Functioning Classifica-tion System (GMFCS) more than level IV (OR=1.480 ; 95%% CI 1.184 to 1.850 ; P!0.006). Conclusion : Pneumonia, AKI and severe GMFCS level were risk factors of death in patients with CP. J. Med. Invest. 65 : 18-20, February, 2018
Keywords : Mortality risk factor, Children, Cerebral Palsy, Indonesia
Received for publication May 17, 2017 ; accepted June 12, 2017. Address correspondence and reprint requests to dr. Prastiya Indra Gunawan, SpA, Pediatric Neurology Staff, Depatment of Child Health, Airlangga University College of Medicine, Jl. Prof Dr Moestopo 6 - 8 Surabaya Indonesia and Fax : +62 - 31 - 5501748.
The Journal of Medical Investigation Vol. 65 2018
18
less than 0.05 were considered to indicate statistical significance. Ethics
Ethics approval was sought from the Ethic and Medico - legal Committee at Dr. Soetomo Hospital and Airlangga University Surabaya. Consent waiver was obtained from the Ethics and Medico - legal Committee at Dr. Soetomo Hospital for the evalu-ation of the medical record data.
RESULTS
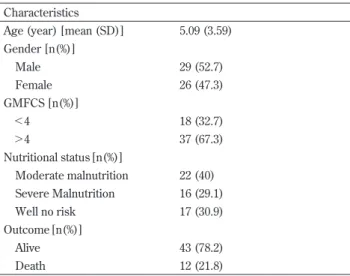
Fifty five children with cerebral palsy were enrolled in this study. The outcome of this study saw 12 patients (21.8%) who had died and 43 patients (78.2%) who were alive.
The risk factor of mortality in cerebral palsy is shown in table 2. Pneumonia was the most common underlying disease cause of death (Odd’s Ratio (OR) = 5.185 ; 95% Confidence Interval (CI) 1.249 to 21.520 ; P!0.007) followed by Acute Kidney Injury (AKI) (OR = 3.333 ; 95% CI 1.317 to 8.436 ; P!0.03). According to the Gross Motor Functioning Classification System (GMFCS) cere-bral palsy is more than level IV determined for severe disability. GMFCS was also significant for the risk of mortality (OR = 1.480 ; 95% CI 1.184 to 1.850 ; P!0.006).
Discussion
CP is the most common and serious disability affecting children, it may also be at least a contributory cause of death more often than is currently certified. The lack of published routine data on CP in Indonesia including their life expectancy emphasises the crucial contribution of well maintained CP registers to provide information that complements mortality data and can be extrapolated nationally (2).
The infant mortality rate in Indonesia was 23 per 1000 live birth in 2015 (8). CP was not mentioned at all in the cause of death state-ment of 45% of those who died, but it was more likely to be the underlying cause of death with increasingly severe disability. There was no clear time trend in the pattern of certifying cerebral palsy, but more time needs to elapse to confirm if there really was a more recent, increasing tendency to include CP in the cause of death statement (9).
It is well known that individuals with CP are subject to higher mortality than the general population but the causes of this have not been systematically analyzed. Several mortality factors have been investigated, otherwise only three risk factors were statistically sig-nificant. The most common underlying cause of death in current research was pneumonia. There was no consecutive pattern in late impairment CP. However, in early impairment CP, other respira-tory conditions (mostly inflammarespira-tory ; 8.8%), and a comparable proportion for combined “other cerebral degenerations” or “other congenital anomalies of nervous system” (both including hydro-cephalus), were jointly the next most common underlying cause of death (table 2). Respiratory disease is known to be a leading cause of death among individuals with cerebral palsy (10).
According to Strauss, the standardized mortality ratio in CP due to respiratory diseases was very high but, contrary to anecdotal reports, such diseases did not account for most deaths (10). Reddihoughet al., and Baird et al., observed respiratory problems, such as pneumonia to be most commonly reported causes of death in CP (12, 13). Tapinet al., stated that among the principal causes of mortality noted in their sample, the primary cause of death was represented by the category “symptoms, signs and ab-normal clinical and laboratory findings, not classified elsewhere” (ICD- 10 codes R00 to R99). In this category, respiratory and circulatory causes were found to be the most common, comprising of two -thirds of all cases. This was followed by “diseases of the respiratory system”, with a mortality rate of 19% compared with 6% in the French general population, a finding which concurred with other published data (14).
Acute kidney injury was considered the second most common cause of death in current research. A recent multinational pro-spective study called as the Assessment of Worldwide Acute Kidney Injury, Renal Angina, and Epidemiology (AWARE) study, involving 4,683 critically ill children revealed that AKI developed in 1,261 (26.9%) patients during the first week of ICU admission. Severe AKI occurred in 543 (11.6%) patients and is related to an increased risk of death by day 28, increased use and duration of mechanical ventilation and renal replacement therapy. Respiratory and neurologic disorders stood out as the first (38.7%) and second (35.2%) most common co - existing conditions in the critically ill children in this study (15). Therefore, it fits the pattern of AKI development in this study on critically ill children with cerebral palsy. The presence of any chronic systemic diseases is proven to contribute to AKI in adult studies. Cerebral palsy is a significant chronic condition in children that affects multiple organs systemi-cally when in critical condition. Several risk factors were associated with severe AKI including transplantation, decreased renal perfu-sion, the use of nephrotoxic medications, radiocontrast exposure, poor nutrition and glycemic control, and major surgery as the most common findings(15 - 17). However, the AWARE study data Table 1. Baseline characteristics
Characteristics
Age (year) [mean (SD)] 5.09 (3.59) Gender [n(%)] Male 29 (52.7) Female 26 (47.3) GMFCS [n(%)] !4 18 (32.7) "4 37 (67.3) Nutritional status [n(%)] Moderate malnutrition 22 (40) Severe Malnutrition 16 (29.1) Well no risk 17 (30.9) Outcome [n(%)] Alive 43 (78.2) Death 12 (21.8)
Table2. Risk factor of mortality
Subject Sig. OR 95%CI Pneumonia 0.007* 5.185 1.249 - 21.52 AKI 0.030* 3.333 1.317 - 8.436 GMFCS 0.006* 1.480 1.184 - 1.850 Acute Diarrhea 0.326 0.262 0.015 - 4.529 Meningoencephalitis 0.489 0.583 0.493 - 4.563 Epilepsy 0.108 3.143 0.747 - 13.22 Subdural hygroma 0.273 1.308 1.123 - 1.523 Leukemia 0.056 4.909 2.897 - 8.318 Sepsis 0.077 0.225 0.039 - 1.303 Hypothyroidism 0.326 0.262 0.015 - 4.529 Pulmonary Tuberculosis 0.149 0.308 0.058 - 1.623 Communicating hydrocephalus 0.170 1.324 1.129 - 1.553
*statistically significant using logistic regression.
suggested that children are more likely to survive severe AKI than adults due to greater renal reserves in children (15). It is to be noted that AKI survivor children are at risk for chronic kidney disease, long - term follow - up is warranted.
As mortality rates in children with CP vary strongly with the severity of disabilities, for modeling purposes the data was divided into 2 groups : mild to moderate (GMFCS I through III) and severe (GMFCS levels IV and V). GMFCS was considered the third significant factor of mortality in CP in this research. Brookset al., stated for CP patientswith body weights below the 20thpercentile
and GMFCS levels III through V, they were related with a mortality hazard ratio of 1.5 (95% confidence interval) (18). Children with CP who have very low weights have more major medical conditions and are at increased risk of death. The life expectancy of CP pa-tients is associated with the type and severity of motor disability. Severe quadriplegia has been associated with a decreased life expectancy. Other significant variables include related disabili-ties and availability of quality medical care. The risk of death is highest in the first 5 years of life. As mortality data is already available, it is now clear that with reasonable medical attention, a majority of affected persons will survive into adult life. A number of factors affect the prognosis of the child with cerebral palsy : the clinical type of cerebral palsy, the degree of delay in meeting mile-stones noted at evaluation, the pathologic reflexes present as de-scribed above, and the degree of associated deficits in intelligence, sensation, and emotional adjustment (11, 19).
This study had a number of important limitations. Firstly, the ab-sence of epidemiological data about the CP population in Indonesia meant it was impossible to accurately determine the number of subjects with CP. A further limitation comprised of the data collec-tion method which used only death certificates, as this allowed only incomplete data to be extracted and other studies have identified this source as a weakness.
CONCLUSION
CP is a chronic condition with considerable impact on affected individuals. Overall prevention of CP has not been successful. Current research has found that pneumonia, AKI and severe GMFCS levels were risk factors of death in patients with CP. Large epidemiological studies such as this deal only with gross patterns, and leave many unanswered questions. It is therefore hoped that the findings will stimulate more focused research on the reasons for excess mortality in CP.
CONFLICT OF INTEREST
The authors declare there is no conflict of interest.
ACKNOWLEDGEMENT
The authors would thank to Mrs Nur Fitriyah for helping data collection.
REFERENCES
1. Mutch L, Alberman E, Hagberg B, Kodama K, Perat MV : Cerebral palsy epidemiology : where are we now and where are we going? Dev Med Child Neurol 34 : 547 - 51, 1992 2. Rosen MG, Dickinson JC : The incidence of cerebral palsy.
Am J Obstet Gynecol 167 : 417 - 23, 1992
3. MacLennan A : A template for defining a causal relation be-tween acute intrapartum events and cerebral palsy : interna-tional consensus statement. BMJ 319 : 1054 - 9, 1999 4. Palisano RJ, Rosenbaum PL, Walter Set al : Development and
reliability of a system to classify gross motor function in child with cerebral palsy. Dev Med Child Neurol 39 : 214 - 23, 1997 5. Tsirikos Al, Chang WN, Dabney KW, Miller F, Glutting : Life
expectancy in pediatric patients with Cerebral palsy and neuromuscular scoliosis who underwent spinal fusion. Dev Med Child 45 : 677 - 82, 2003
6. Hollins S, Attard MT, von Fraunhofer N, McGJKuigan S, Sedgwick P : Mortality in people with learning disability : risks, causes, and death certification findings in London. Dev Med & Child Neu 40 : 50 - 6, 1999
7. Plioplys AV, Kasnicka I, Lewis S, Moller D : Survival rates among children with severe neurologic disabilities. Southern Medical Journal 91 : 161 - 72, 1998
8. The World Bank : Infant mortality rate in Indonesia 2015. Available at : http : //data.worldbank.org/indicator/SP. DYN.IMRT.IN?locations = ID (accessed on 12 June 2017) 9. Maudsley G, Hutton JL, Pharoah P : Cause of death in
cere-bral palsy : a descriptive study. Arch Dis Child 81 : 390 - 4, 1999
10. Strauss DJ : Life expectancy of children with cerebral palsy. Dev Med & Child Neu. Lancet 349 : 263 - 4, 1997
11. Strauss D, Cable W, Shavelle R : Causes of excess mortality in cerebral palsy. Dev med & Child Neurol 41 : 580 - 5, 1999 12. Baird G, Allen E, Scrutton D, Knight A, McNee A, Will E,
Elbourne D : Mortality from 1 to 16 - 18 years in bilateral cere-bral palsy. Arch Dis Child 96 : 1077 - 81, 2011
13. Reddihough DS, Bikie G, Walstab JE : Cerebral palsy in Victoria, Australia : mortality and causes of death. J Paedtr Child Health 37(2) : 183 - 6, 2001
14. Tapin AD, Colin A, Nicolas B, Lebreton C, Dauvergne F, Gallein P : Analysis of the medical causes of death in cerebral palsy. Ann of Phys and Rehab Med 57(1) : 24 - 37, 2014 15. Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL :
Epide-miology of acute kidney injury in critically ill children and young adults. NEJM 376(1) : 11 - 20, 2017
16. Chertow GM, Burdick E, Honour M, Bonventre JV, David WB : Acute kidney injury, mortality, length of stay, and cost in hospitalized patients. J Am Soc Nephrol 16 : 3365 - 70, 2005 17. Kellum JA, Sileanu FE, Murugan R, Lucko N, Shaw AD,
Clermont G : Classifying AKI by urine output versus serum creatinine level. J Am Soc Nephrol 26 : 2231 - 8, 2015 18. Brooks J, Day S, Shavelle R, Strauss D : Low birth weight,
morbidity and mortality in children with cerebral palsy : new clinical growth charts. Pediatrics 128(2) : e299 - 307, 2011 19. Holmes L, Joshi A, Lorenz Z, Miller F, Debney K, Connor Jet
al : Pediatric cerebral palsy life expectancy : has survival im-proved over time? Pediat Therapeut 3(1) : 1 - 6, 2013