INTRODUCTION
Abdominal malignancies, such as colorectal cancer or pancreatic cancer, remain being the leading causes of cancer-related deaths in the world. Despite many multidisciplinary advances in cancer treatment, complete surgical removal at early stage of diseases still remains the only
potential curative treatment for the majority of the abdominal malignancies. Therefore, early detection of tumors, ideally before clinical symp-toms develop, is the most important to poten-tially decrease the mortality. Although the recent evolution of diagnostic technology, such as multi-detector-row computed tomography (MDCT) or fast magnetic resonance (MR) imaging, has changed the landscape of oncologic imaging, not a few patients remain amenable to surgical resection despite their advanced stage even at the fi rst documentation of the disease. In the light of such insuffi cient diagnostic performance
High-B-Value Diffusion-Weighted MR Imaging of Body:
Clinical Usefulness for Detecting Malignant Tumors
Katsuhiro SANO1), 2)*, Tomoaki ICHIKAWA1), 2), Utaroh MOTOSUGI1), Tsutomu ARAKI1) 1) Department of Radiology, University of Yamanashi, Yamanashi, Japan
2) Department of Diagnostic Radiology, Saitama Medical University
International Medical Center, Saitama, Japan
Abstract: Purpose: Primary outcome of this study was to compare the detectability of
high-b-value Diffusion-weighted MR imaging (DWI) with those of conventional (unen-hanced T1WI and T2WI) MR imaging and contrast-en(unen-hanced multidetector-row com-puted tomography (CE-MDCT) for malignancies of the body. Interpretation time for each image was also determined as a secondary outcome.
Materials and Methods: 253 patients with 273 malignant tumors and 278 patients with-out malignant tumors were included in this study. Three examiner separately reviewed the 4 sets of images; 1. CE-MDCT, 2. high-b-value DWI series alone, 3. conventional MRI and 4. high-b-value DWI + conventional MRI. In addition, the examiners record-ed their interpretation times for each image set. Az value was calculatrecord-ed by ROC analysis. Results: The mean Az values of CE-MDCT, high-b-value DWI alone, conventional MRI, and high-b-value DWI + conventional MRI were 0.82, 0.85, 0.90 and 0.95 respectively. The mean interpretation time for high-b-value DWI alone was signifi cantly shorter than those of the other image sets.
Conclusion: High-b-value DWI in addition to conventional MR imaging contributes to improving diagnostic ability of detecting of abdominal and pelvic malignancies without extending interpretation time.
Key Words: magnetic resonance imaging, diffusion weighted imaging, high-b-value, malignant tumor
Original article
* C o r r e s p o n d i n g a u t h o r : K a t s u h i r o S a n o , Department of Radiology, University of Yamanashi, 1110 Shimokato, Chuo-city, Yamanashi 409-3898, Japan.
Received September 30, 2016 Accepted November 29, 2016
with the morphology-based imaging techniques, there is now a compelling need for establishing a new imaging technique as a cancer-screening method to provide suffi ciently high sensitivity for all kinds of abdominal malignancies.
It is well known that diffusion is caused by random translational molecular motion, known as Brownian motion. MR imaging is the only method that can evaluate the diffusion process
in vivo1). Therefore, diffusion-weighted (DW) MR
imaging (DWI) is quite different from the mor-phologically-oriented imaging techniques, since DWI can detect disease-associated changes in the random diffusion. Based on this character-istic of DWI, DWI is effectively used as a highly sensitive imaging modality in the early detection of cerebral infarction2). Moreover, several inves-tigators recently reported that quantifi cation of diffusion by apparent diffusion coeffi cient (ADC) values is useful for differentiating be-tween benign and malignant lesions in many or-gans, such as breast3), liver4, 5), kidney6), ovary7), or prostate8). In fact, although DWI might be considered as a promising imaging technique in the evaluation of malignant lesions, the standard application of DWI is not qualitative but quanti-tative and based on time-consuming ADC meas-urements. Consequently, DWI has been recog-nized as a sophisticated technique and its ability to detect early malignancy in the clinical setting has also been neglected.
Takahara et al.9, 10) proposed a DWI technique that might provide images with improved signal-to-noise ratios (SNRs); reversal of the contrast of these images resulted in black-on-white images with contrast characteristics closely resembling those of positron emission tomography (PET). More recently, Ichikawa et al.11, 12) reported that direct visual assessment of high-b-value DW im-ages has a high sensitivity and specifi city in the detection of colorectal cancer and pancreatic
cancer.
Recently, image interpretation time for the radiologists has been explosively extended be-cause of increasing numbers of examinations and slices of MDCT and fast MRI on a daily basis. Exhausted radiologists have been thirsty for a new imaging technique that can effectively make interpretation time shorter without dimin-ishing the excellent lesion sensitivity.
Can high-b-value DWI realize the excellent le-sion sensitivity with only short image interpreta-tion time in the detecinterpreta-tion of comprehensive ma-lignancies throughout the body? The purpose of this study was to evaluate high-b-value DWI as a diagnostic tool for depicting abdominal and pel-vic malignancies using direct visual assessment of the obtained images, and to compare the di-agnostic performance and image interpretation time of high-b-vale DWI with those of contrast-enhanced MDCT (CE-MDCT) and uncontrast-enhanced T1-weighted image and T2-weighted image (conventional MRI) in the detection of abdomi-nal and pelvic malignancies.
MATERIALSANDMETHODS
A. Patients
During the period of 41 months between Au-gust 2004 and December 2007, 531 consecutive patients (mean age, 56.5 years; range, 12–90 years; 351 women, 180 men) consisting of 253 patients with 273 malignant tumors and 278 pa-tients without malignant tumors were included in this study. Malignant tumors ranging from 5 to 120 mm (mean, 27.6 mm) in diameter were detected in our institution and two associated hospitals and were included in this study. The lesions were located in the liver (n = 46; 21 hepa-tocellular carcinomas, 1 intrahepatic cholangio-carcinoma, 24 metastatic tumors), pancreas (n = 39; 39 invasive ductal adenocarcinomas),
com-mon bile duct (n = 5; 5 cholangiocarcinomas), gallbladder (n = 4; 4 gallbladder carcinomas), kidney (n = 4; 4 renal cell carcinomas), and stomach (n = 4; 4 gastric carcinomas) in the up-per abdomen. And the lesions were located in the colorectum (n = 59; 59 colorectal carcino-mas), prostate (n = 30; 30 prostatic carcinoma), ovary (n = 37; 37 ovarian carcinomas), uterus (n = 40; 25 uterine cervical carcinomas, 15 endo-metrial carcinomas), bladder (n = 2; 2 urothelial carcinomas) and abdominal wall (n = 3; 3 peri-toneal carcinomas) in the pelvis. The diagnoses of malignant tumors were confi rmed by pathol-ogy obtained by surgical resection or biopsy, or fi ndings on the clinical follow-up examinations by multi-imaging modalities. CE-MDCT was performed in all patients before MR examina-tions. Informed consent was obtained from each patient before participation in the study.
B. Imaging Protocol and Analysis 1. Imaging Protocol
All MRI examinations were performed using commercially available 1.5-T superconducting 2 MR units (Signa Excite HD, GE Healthcare, Milwaukee, USA and Intera Nova Dual, Philips Medical Systems, Amsterdam, Netherland). First, breath-hold fat-saturated T1-weighted MR images were obtained with a combination of gradient-echo sequences and chemical shift se-lective fat-suppression techniques (TR range/TE range, 150–170 ms/2–4.6 ms; matrix, 240×192; reduction factor (SENSE and ASSET), 2). Sec-ond, respiratory-triggered fat-saturated T2-weighted fast spin-echo images were acquired (TR range/TE, 1,000–7,000 ms/70–75 ms; echo-train length, 8–12; matrix, 320×256; reduc-tion factor (SENSE and ASSET), 2). Contrast-enhanced MR images were obtained after bolus injection of 0.2 mL/kg of gadopentetate dimeg-lumine (Magnevist, Schering, Berlin, Germany).
Finally, all patients underwent DWI using the body coil of the MR unit. The patients did not undergo any preparation such as bowel cleans-ing before the examinations. The DWI tech-nique was a modifi ed version of the original DWI protocol6, 7). The detailed parameters of DWI were as follows: sequence, single-shot spin-echo spin-echo-planar with chemical-shift selective fat-suppression technique; scan direction, axial; respiration, non-breath-hold method; b value, 1,000 s/mm2 (with diffusion weighted gradients applied in three orthogonal directions); TR range/TE range, 4,700–15,000 ms/65–72 ms; in-version time, 70 milliseconds; matrix, 128×64; slice thickness/gap, 4 mm/0 mm; fi eld of view, 400×280 cm; number of excitations, 6; reduc-tion factor (SENSE and ASSET), 2; and ac-quisition time, approximately 5 minutes. All axial source images were provided with black-on-white reversal display to facilitate lesion de-tection. Coronal maximum-intensity-projection (MIP) images were also reconstructed from the axial source images and were evaluated using a 3D rotational cine mode. All CT images were ob-tained by 16-detector-row MDCT systems (Bril-liance 16, Philips Medical Systems, Amsterdam, Netherland and Aquilion 16, Toshiba Medical Systems, Tokyo, Japan). The parameters were as follows, detector row, 2 mm; reconstructed slice thickness, 5 mm. All patients were admin-istered by 600 mgI/kg of non-ionic iodine con-trast agent. Injection time of concon-trast agents was 50 sec and scan delay was 90 sec.
2. Imaging Analysis
The primary outcome of this study was to compare the detectability of high-b-value DWI with those of conventional MR imaging and CE-MDCT for malignancies of the body. We also de-termined the difference of image interpretation time for each group as the secondary outcome.
On the basis of pathologic results and clinical follow up examinations, two coordinators at-tempted to determine the location of the lesions and to anatomically correlate the pathologically confi rmed lesions with the imaging fi ndings as accurately as possible to allow detection of false-positive interpretations. The coordinators had access to all imaging, clinical, and surgical data of the patients and control subjects. All high-b-value DW images were then independently interpreted in random order and blinded fash-ion by three off-site examiners (abdominal radi-ologists with 7, 9, and 21 years of experience, respectively) other than the coordinators. The examiners were aware that the study was being performed to detect malignant tumors. How-ever, they were blinded to the other data, such as patient identity, clinical history, the fi ndings of other imaging examinations, and results of histopathologic evaluations. The examiners sep-arately reviewed the 4 sets of images in the fol-lowing order; 1. CE-MDCT, 2. high-b-value DW image series alone, including axial source and MIP images without referring to any other MR images, 3. conventional MRI and 4. high-b-value DWI + conventional MRI. Interpretation time for each image set was measured. MIP images were evaluated with the rotational cine mode to-gether with the axial source images in different windows on diagnostic monitors. Each examiner graded the presence (or absence) of lesions on a 5-grade confi dence scale on the basis of the strength and appearance of dark signals on the high-b-value DW images as follows: 1, defi nitely absent (no signal); 2, probably absent (nonlocal-ized, mild to moderate signal); 3, undetermined (localized, mild to moderate signal); 4, probably present (localized, strong signal with poorly de-fi ned margins); and 5, dede-fi nitely present (local-ized, strong signal with well-defi ned margins). If a lesion was considered to be present on these
images, the location of the lesion was recorded. Only lesions recorded at the correct location de-termined by the coordinators were accepted as true-positive fi ndings. In addition, the examin-ers recorded their interpretation times for each imaging technique.
C. Statistical Analysis
Receiver operating characteristic (ROC) curves were used to represent the performance of in-dividual examiners for tumor detection. The diagnostic accuracy for each examiner was de-termined by calculating the area under the ROC curve (Az). Sensitivity and specifi city were also calculated with defi nition of Grade 4 and 5 as positive for the presence of malignant tumor. In the study of diagnostic performance for the detection of lymph node metastases and peri-toneal disseminations, Az value, sensitivity and positive predictive value (PPV) were also calcu-lated. The interobserver agreement among ex-aminers for tumor detection was calculated with linearweighted kappa statistics. A kappa statistic greater than 0.75 was considered to indicate excellent agreement beyond chance; 0.4–0.75, fair to good agreement; and less than 0.4, poor agreement13).
RESULTS
Primary outcome: comparison of detectability (main table: Table 1)
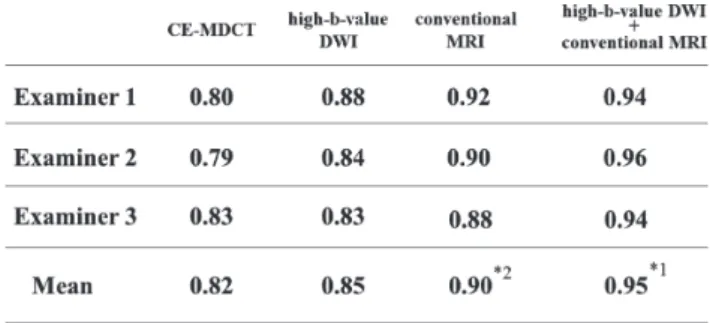
The Az values of each image set for three ex-aminers were shown on Table 1. ROC analysis yielded mean Az values of 0.82 for CE-MDCT, 0.85 for high-b-value DWI alone, 0.90 for con-ventional MRI and 0.95 for high-b-value DWI + conventional MRI. The mean Az value of high-b-value DWI + conventional MRI was signifi cantly higher than those of the other image sets. And the mean Az value of conventional MRI was
sig-nifi cantly higher than those of CE-MDCT and high-b-value DWI alone. ROC curves for detect-ing malignant tumors were shown in the Fig. 1. In the same way, the mean sensitivities were 62% (167/268) of CE-MDCT, 79% (215/273) of high-b value DWI alone, 72% (198/173) of
convention-al MRI, 87% (237/273) of high-b-vconvention-alue DWI + conventional MRI, respectively. The sensitivity of high-b-value DWI + conventional MRI was signifi cantly higher than those of the other im-age sets. And the sensitivity of contrast-enhanced MDCT was signifi cantly lower than those of the Fig. 1. ROC curves for detecting of abdominal and pelvic malignancies.
The mean Az value with diffusion-weighted imaging +conventional MR imaging was signifi cantly higher than those with the other techniques. Table 1. Az values for detection of abdominal and pelvic malignancies
Az values for detection of abdominal and pelvic malignancies using each technique. *1 Az value of high-b-value DWI+conventional MRI was signifi cantly higher than that of other techniques (p < 0.008). *2 Az value of conventional MRI was signifi cantly higher than that of CE-MDCT and high-b-value DWI alone (p < 0.008).
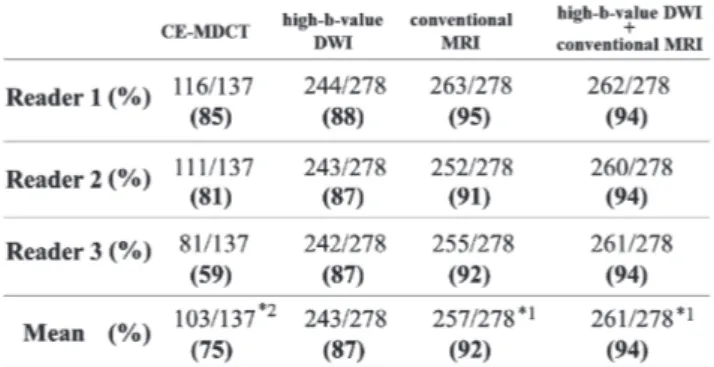
other image sets (Table 2). The mean specifi cities of CE-MDCT, high-b-value DWI alone, tional MRI, and high-b-value DWI + conven-tional MRI were 75% (103/137), 87% (243/278), 92% (257/278) and 94% (261/278), respectively. The specifi cities of conventional MRI and high-b-value DWI + conventional MRI were sig-nifi cantly higher than those of CE-MDCT and high-b-value DWI alone. And the specifi city of contrast-enhanced MDCT was signifi cantly low-er than those of the othlow-er image sets (Table 3).
The sensitivities of malignant tumors for each organ were as follows. The mean sensitivities for hepatocellular carcinoma were 62% (13/21) for CE-MDCT, 43% (9/21) for high-b-value DWI alone, 67% (14/21) for conventional MRI, 76% (16/21) for high-b-value DWI + conventional MRI, respectively. The sensitivity of high-b-value DWI alone was signifi cantly lower than those of the other image sets (Table 4). In the same way, the mean sensitivities for metastatic
liver tumor were 88% (21/24), 83% (20/24), 88% (21/24) and 92% (22/24) for each image set, respectively. There were no signifi cant dif-ferences among these image sets (Table 4). The mean sensitivities for gallbladder carcinoma and cholangiocarcinoma were 78% (7/9), 89% (8/9), 78% (7/9) and 89% (8/9) for each image set, respectively. There were no signifi cant dif-ferences among these image sets (Table 4). The mean sensitivities for pancreatic adenocarcino-ma were 92% (36/39), 87% (34/39), 90% (35/39) and 95% (37/39) for each image set, respectively. There were no signifi cant differences among these image sets (Table 4). The mean sensitivi-ties for gastric carcinoma were 25% (1/4), 50% (2/4), 50% (2/4) and 50% (2/4) for each image set, respectively. The sensitivity of CE-MDCT was signifi cantly lower than those of the other image sets (Table 4). The mean sensitivities for colorec-tal carcinoma were 63% (37/59), 80% (47/59), 49% (29/59) and 85% (50/59) for each image Table 2. Sensitivities for detection of abdominal and pelvic malignancies
Sensitivities for detection of abdominal and pelvic malignancies using each technique. *1 Sensitivity of high-b-value DWI+conventional MRI was signifi cantly higher than that of other techniques (p < 0.008). *2 Sensitivity of CE-MDCT was signifi cantly lower than that other techniques (p < 0.008).
set, respectively. The sensitivities of CE-MDCT and conventional MRI were signifi cantly lower than those of the other image sets (Table 5). The mean sensitivities for uterine malignant tumors were 58% (23/40), 83% (33/40), 83% (33/40) and
85% (34/40) for each image set, respectively. The sensitivity of CE-MDCT was signifi cantly lower than those of the other image sets (Table 5). The mean sensitivities for ovarian malignant tumors were 63% (20/32), 87% (32/37), 87% (32/37) and Table 3. Specifi cities for detection of abdominal and pelvic malignancies
Specifi cities for detection of abdominal and pelvic malignancies using each technique. *1 Specifi city of high-b-value DWI+conventional MRI was signifi cantly higher than that of high-b-value DWI (p < 0.008). *2 Specifi cities of CE-MDCT was signifi cantly lower than those ofother image sets (p < 0.08).
Table 4. Mean sensitivities for individual upper abdominal malignancies
Mean sensitivities for individual upper abdominal malignancies us-ing each technique. *Mean sensitivities for hepatocellular carcinomas of high-b-value DWI and for gastric cancer of CE-MDCT were sig-nifi cantly lower than those of other techniques.
87% (32/37) for each image set, respectively. The sensitivity of CE-MDCT was signifi cantly lower than those of the other image sets (Table 5). The mean sensitivities for prostatic carcino-ma were 7% (2/30), 23% (7/30), 20% (6/30) and 33% (10/30) for each image set, respectively. The sensitivity of high-b-value DWI + conventional MRI was signifi cantly higher than those of the other image sets (Table 5). All values indicating interobserver agreement were in the category of excellent (κ = 0.81–0.87).
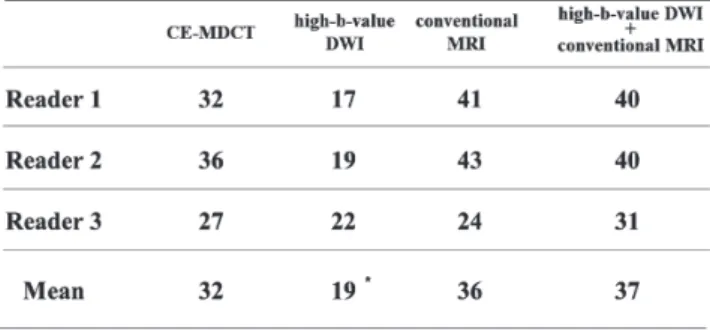
Secondary outcome: comparison of interpretation time (Table 6)
Interpretation times (sec) leading up to fi nal diagnosis were shown on the Table 6. The mean interpretation time for high-b-value DWI alone was 19 sec which was signifi cantly shorter than those of the other image sets (CE-MDCT 32 sec, conventional MRI 36 sec, high-b-value DWI + conventional MRI 37 sec). There were no sig-nifi cant differences in the mean interpretation
time among CE-MDCT, conventional MRI and high-b-value DWI + conventional MRI.
DISCUSSION
High-b-value DWI was effective for detect-ing almost all types of abdominal malignancies. However, some types of malignancies were dif-fi cult to be detected with DWI because of the absence of signifi cantly high signal of the tumor, respiratory or peristaltic motion-artifacts, or the strong signals produced by the surrounding normal tissues.
The best indication of high-b-value DWI in the upper abdomen might be the detec-tion of hepatic metastases (Fig. 2), biliary can-cers, pancreatic cancan-cers, or colon cancers11, 12). Identifi cation of gastroduodenal/biliary tract lesions on high-b-value DWI may depend on the acquisition techniques because respiratory/ peristaltic motion artifacts signifi cantly affect the visualization of the lesions. Therefore, respira-Table 5. Mean sensitivities for individual pelvic malignancies
Mean sensitivities for individual pelvic malignancies using each technique. Mean sensitivities for all malignancies of high-b-value DWI+conventional MRI were higher than those with CE-MDCT. In addition, mean sensitivities for pelvic malignancies except ovarian malignancies of high-b-value DWI+conventional MRI were partially higher than those of high-b-value DWI and conventional MRI.
tory-triggered techniques for high-b-value DWI should be fi nally required for detecting upper abdominal malignancies. High-b-value DWI for detecting hepatocellular carcinoma (HCC) may be still challenging. The identifi cation of HCC with high-b-value DWI may depends on rela-tively high signals of the cirrhotic liver as a back-ground and the differentiation of the tumors; the sensitivity for well-differentiated HCC is not so high as that for
moderately/poorly-differenti-ated ones.
High-b-value DWI has a defi nite advantage over 18F-labeled analog of glucose, 2’-deoxy-2’-[18F]fl uoro-D-glucose PET (FDG-PET) for eval-uating pelvic cavity. Indeed, exploration in the pelvic cavity with FDG-PET may be impossible due to strong signals produced in the urinary bladder. The best indication of high-b-value DWI in the pelvis might be the detection of colo-rectal cancers, uterine cervical cancers, ovarian Table 6. Interpretation time (sec) leading up to fi nal diagnosis
The interpretation time for each technique. Interpretation time for high-b-value DWI was signifi cantly shorter than those of other tech-niques. Interpretation time was not prolonged by adding high-b-value DWI to conventional MRI.
Fig. 2. A: fat-saturated T2WI, B: high b-value DWI
Liver metastasis (with bone metastases) from esophageal cancer in a 68-year-old man. Fat-saturated T2WI shows a small liver metastasis (Arrow). Additionally, multiple hy-perintense lesions are demonstrated in the vertebral bone (Circle). Both the liver and bone metastases are more clearly depicted on high-b-value DWI.
cancers (Fig. 3), or bladder tumors followed by prostate cancers. For pelvic malignancies, cervi-cal, some of small ovarian cancers and uterine endometrial cancers might not be detected be-cause normal ovary and uterine endometrium always show high signals similar to those of ma-lignancies. However, high-b-value DWI is effec-tive for staging of ovarian cancers because high-b-value DWI is sensitive for detecting peritoneal disseminations (Fig. 3).
High-b-value DWI for detecting prostate can-cers is still challenging. Indeed, high-b-value DWI may not improve the sensitivity of T2WI for prostate cancers arising from peripheral zone (PZ). However, detectability of cancers arising from transitional zone (TZ) can be im-proved with high-b-value DWI combined with
T2WI. The visualization of prostate cancers may be obscured by high signals of the normal pros-tate or benign prostatic hypertrophy (BPH) as a background similar to that of the lesions. A use of higher b-value (e.g., 2,000 sec/mm2) may im-prove the differentiation between cancers and normal prostate or BPH.
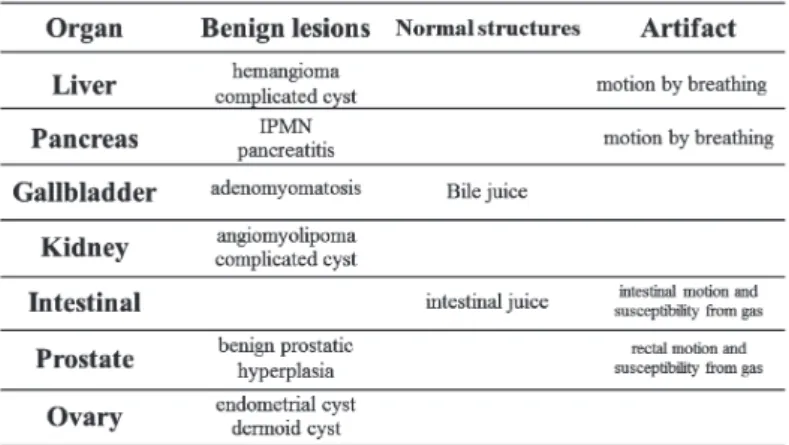
Normal organs such as endoreticular organs (spleen, lymph node), prostate, seminal vesicle, uterine endometrium, ovary, or contents in the alimentary tract might exceptionally show high signals on high-b-value DWI because of their low ADC or high T2 values. In addition, it should be recognized that some benign conditions, such as benign neoplasms or active infl ammation, may show high signals. Such phenomenon might de-pend on hypercellularity14, 15), viscosity (myxoid Fig. 3. A: T2WI coronal image, B, C: T2WI axial image, D: high b-value DWI coronal image,
E, F: high b-value DWI axial image
Serous cystadenocarcinoma of ovary in a 74-year-old woman. Multiple mural nodules (white arrows) in the tumor show strong signals regardless of their size. Each peritoneal dissemination (black arrows) is clearly identifi ed as a focal strong signal on high-b-value DWI.
matrix, viscous fl uid, or hemorrhage) or tissue edema in active infl ammation. False-positive cases on DWI are summarized on Table 7. It is important during the interpretation of DWI to keep in mind that some normal tissues or benign conditions frequently show similar strong signals to those of malignancies of the body.
Interpretation time of DWI was signifi cantly shorter than those with the other techniques. This seems to be due to the ‘white-on-black’ inversion images of high-b-value DWI which resemble FDG-PET images, facilitating image interpretation with ‘Yes’ or ‘No’. As a result, ad-dition of DWI to the conventional MR imaging did not extend the interpretation time and the diagnostic ability of the MR imaging was im-proved.
High-b-value DWI has several advantages over other imaging modalities for screening, such as CT or PET. High-b-value DWI is com-pletely non-invasive, and never causes discom-fort or adverse effects to patients such as radia-tion exposure, injecradia-tion of contrast materials, or any iatrogenic complications. Therefore, high-b-value DWI allows tumor screening even in the
population with allergic reaction or past-history of adverse effects of contrast materials. In addi-tion, since the principal technique for the con-ventional DWI is well-established, no specifi c technical skills are required for operators. More-over, no expensive costs for maintaining a specif-ic, large-scale system like a cyclotron for PET are required. Thus, high-b-value DWI might have a potential ability to be the fi rst imaging modality for screening patients with symptoms suggesting malignancies.
Our study has some limitations. First, it was retrospective and performed at only one insti-tution. Thus, we consider our fi ndings prelimi-nary. Second, we only evaluated abdominal and pelvic malignancies. Evaluation of malignancies of other site of the body with high-b-value DWI must be performed in future.
In conclusion, high-b-value DWI in addition to conventional MR imaging contributes to im-proving diagnostic ability of detecting of abdom-inal and pelvic malignancies without extending interpretation time.
Table 7. False positive cases
False positive cases on high-b-value DWI. Normal tissue or benign tumor may show high signal intensity.
REFERENCES
1) Le Bihan D, Turner R, Douek P, Patronas N. Diffusion MR imaging: clinical applications. AJR Am J Roentgenol, 159: 591–599, 1992.
2) Lutsep HL, Albers GW, DeCrespigny A, Kamat GN, Marks MP, Moseley ME. Clinical utility of diffusion-weighted magnetic resonance imaging in the assessment of ischemic stroke. Annals of neurology, 41: 574–580, 1997.
3) Sinha S, Lucas-Quesada FA, Sinha U, DeBruhl N, Bassett LW. In vivo diffusion-weighted MRI of the breast: potential for lesion characterization. J Magn Reson Imaging, 15: 693–704, 2002. 4) Namimoto T, Yamashita Y, Sumi S, Tang Y,
Takahashi M. Focal liver masses: characteriza-tion with diffusion-weighted echo-planar MR imaging. Radiology, 204: 739–744, 1997. 5) Ichikawa T, Haradome H, Hachiya J, Nitatori T,
Araki T. Diffusion-weighted MR imaging with a single-shot echoplanar sequence: detection and characterization of focal hepatic lesions. AJR Am J Roentgenol, 170: 397–402, 1998.
6) Squillaci E, Manenti G, Di Stefano F, Miano R, Strigari L, Simonetti G. Diffusion-weighted MR imaging in the evaluation of renal tumours. Journal of experimental & clinical cancer re-search : CR, 23: 39–45, 2004.
7) Moteki T, Ishizaka H. Diffusion-weighted EPI of cystic ovarian lesions: evaluation of cystic con-tents using apparent diffusion coeffi cients. J Magn Reson Imaging, 12: 1014–1019, 2000. 8) Gibbs P, Tozer DJ, Liney GP, Turnbull LW.
Comparison of quantitative T2 mapping and diffusion-weighted imaging in the normal and
pathologic prostate. Magn Reson Med, 46: 1054–1058, 2001.
9) Takahara T, Imai Y, Yamashita T, Yasuda S, Nasu S, Van Cauteren M. Diffusion weighted whole body imaging with background body signal sup-pression (DWIBS): technical improvement us-ing free breathus-ing, STIR and high resolution 3D display. Radiat Med, 22: 275–282, 2004. 10) Kwee TC, Takahara T, Ochiai R, Nievelstein RA,
Luijten PR. Diffusion-weighted whole-body im-aging with background body signal suppression (DWIBS): features and potential applications in oncology. Eur Radiol, 18: 1937–1952, 2008. 11) Ichikawa T, Erturk SM, Motosugi U, Sou H,
Iino H, Araki T, et al. High-B-value diffusion-weighted MRI in colorectal cancer. AJR Am J Roentgenol, 187: 181–184, 2006.
12) Ichikawa T, Erturk SM, Motosugi U, Sou H, Iino H, Araki T, et al. High-b value diffusion-weighted MRI for detecting pancreatic adenocarcinoma: preliminary results. AJR Am J Roentgenol, 188: 409–414, 2007.
13) Kundel HL, Polansky M. Measurement of observ-er agreement. Radiology, 228: 303–308, 2003. 14) Sugahara T, Korogi Y, Kochi M, Ikushima I,
Shigematu Y, Hirai T, et al. Usefulness of diffu-sion-weighted MRI with echo-planar technique in the evaluation of cellularity in gliomas. J Magn Reson Imaging, 9: 53–60, 1999.
15) Lyng H, Haraldseth O, Rofstad EK. Measure-ment of cell density and necrotic fraction in hu-man melanoma xenografts by diffusion weight-ed magnetic resonance imaging. Magn Reson Med, 43: 828–836, 2000.